Hesperian Health Guides
Chapter 6: Guide for Identifying Disabilities
In the first column of the chart, we list the more noticeable signs of different disabilities.
Some of these signs are found in more than one disability. So in the second column we add other signs that can help you tell apart similar disabilities. The third column names the disability or disabilities that are most likely to have these signs, and is linked to the page in the book. (Where it says WTND and then a number, this refers to the page in Where There Is No Doctor
If you do not find the sign you are looking for in the first column, look for another sign. Or check the signs in the second column.
This chart will help you find out which disabilities a child might have. It is wise to look up each possibility. The first page of each chapter on a disability describes the signs in more detail.
Fortunately, it is not always necessary to know exactly what disability a child has. For example, if a child has developed weakness in his legs and you are not sure of the cause, you can still do a lot to help him. Read the chapters on disabilities that cause similar weakness, and the chapters on other disabilities that the child may have. For this child, you might find useful information in the chapters on contractures, exercises, braces, walking aids or wheelchairs, and many others.
Sometimes it is important to identify the specific disability. Some disabilities require specific medicines or foods—for example, night blindness, rickets, or hypothyroidism. Others urgently need surgery—for example, spina bifida or cleft lip and palate. Others require specific ways of doing therapy or exercises—for example, cerebral palsy. And others need specific precautions to avoid additional problems—for example, spinal cord injury and leprosy. For this reason, it helps to learn as much about the disability as you can. Whenever possible, seek information and advice from more experienced persons. (However, even experts are not always right. Do not follow anyone’s advice without understanding the reasons for doing something, and considering if and why the advice applies to the individual child.)
In addition to this chart, 2 other guides for identifying disabilities are in this book:
GUIDE FOR IDENTIFYING CAUSES OF JOINT PAIN.
GUIDE FOR IDENTIFYING AND TREATING DIFFERENT FORMS OF SEIZURES
(EPILEPSY).
Contents
GUIDE FOR IDENTIFYING DISABILITES
To download a pdf of this chart, click here.
SIGNS PRESENT AT OR SOON AFTER BIRTH
| IF THE CHILD HAS THIS | AND ALSO THIS | HE MAY HAVE | |
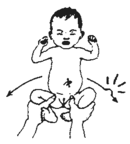
born weak or ‘floppy’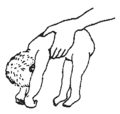 |
|
||
takes longer to begin to lift head or move arms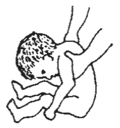 |
|
||
| small head, or small top part of head |  |
||
| none of above | developmental delay for other reasons | ||
does not suck well or chokes on milk or food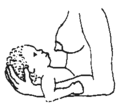 |
|
||
|
| ||
| one or both feet turned in or back | no other signs | club foot | |
 |
 |
||
| dark lump on back | spina bifida | ||
‘bag’ or dark lump on back |
|
spina bifida (sometimes no ‘bag’ is seen, but foot signs may be present) | |
head too big; keeps growing |
may develop: | hydrocephalus (water on the brain) | |
|
At birth, this is usually a sign of spina bifida. | ||
| in an older child, possibly tapeworm in brain, or a brain tumor WTND page 143 | |||
upper lip and/or roof of mouth incomplete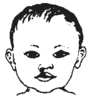 |
|
 |
cleft lip and cleft palate |
| disabilities at birth limbs, fingers or toes not typical |
(may or may not be associated with other problems) |
See | |
 | |||
| unusual stiffness or position |
|
arthrogryposis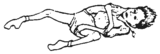 | |
 |
 |
spastic cerebral palsy
| |
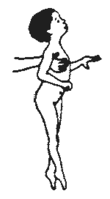
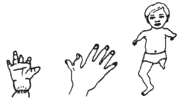
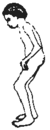
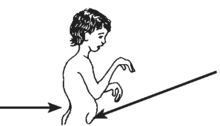
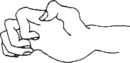
one arm weak or in unusual position |
does not move the arm much holds it like this.  |
Erb’s palsy (weakness from injury to nerves in shoulder during birth) | |
| leg on same side often affected | hemiplegic (one-sided) cerebral palsy | ||
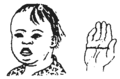
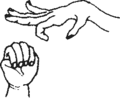
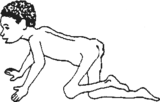
| dislocated hip at birth | On opening legs like this, leg ‘pops’ into place or does not open as far. | dislocated hip from birth (often both hips) may be present with: | |
 leg held differently, shorter; flap covers part of vulva |
 |
 |
arthrogryposis Also see Hip Problems |
slow to respond to sound or to look at things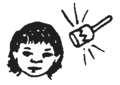 |
(may be due to one or a combination of conditions) |
Check for signs of: | |
SIGNS IN CHILDREN
| IF THE CHILD HAS THIS | AND ALSO THIS | HE MAY HAVE | ||
| delayed in most or all areas: | developmental delay, check for signs of: | |||
takes longer than other children to do things (roll, sit, use hands, show interest, walk, talk)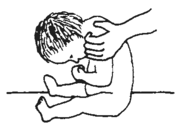 |
 |
Down syndrome | ||
 |
hypothyroidism | |||
has continuous unusual movements or positions, and/or stiffness |
cerebral palsy also check for: | |||
| does not respond to sounds, does not begin to speak by age 3 | may respond to some sounds but not others Check for ear infection (pus). |
Check for
| ||
 | ||||
| does not turn head to look at things, or reach for things until they touch her | Eyes may or may not look typical. |
| ||
 | ||||
| Eyelids or eyes make quick, jerky, or strange movements. |  |
Check for one or a combination of these | ||
| All or part of body makes strange, uncontrolled movements. |
|
epileptic seizures (Pattern varies a lot in different children—or even in the same child.) | ||
 |
slow sudden, or rhythmic movements; fairly continuous (except in sleep); no loss of consciousness |
athetoid cerebral palsy (Note: Seizures and cerebral palsy may occur in the same child.) | ||
| Body, or parts of it, stiffens when in certain positions: difficulty with control of some or all movements. |
|
spastic cerebral palsy | ||
PARTS OF BODY WEAK OR PARALYZED
| IF THE CHILD HAS THIS | AND ALSO THIS | HE MAY HAVE | ||||
| floppy or limp weakness in part or all of body no loss of feeling in affected parts no spasticity (muscles that tighten without control) typical at birth |
 |
polio | ||||
|
 |
|||||
|
tick paralysis | |||||
| paralysis from pesticides, chemicals, foods (lathyrism) | ||||||
| lump on back | tuberculosis of spine | |||||
| floppy or limp weakness usually some loss of feeling |
 |
leprosy | ||||
 |
spina bifida  | |||||
|
spinal cord injury paraplegia (lower body) quadriplegia (upper and lower body) |
 | ||||
 | ||||||
| injury to nerves going to one part of body | hand weakness sometimes caused by using crutches wrongly | |||||
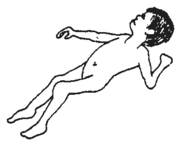
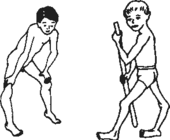
| weakness usually with stiffness or spasticity of muscles no loss of feeling |
usually affects body in one of these patterns |
| ||||
1.
2.
3. |
||||||
| one side |
both legs |
whole body | ||||
| Muscles tighten and resist movement because of joint pain. | JOINT PAIN (many causes—see below) | |||||
JOINT PAIN
| IF THE CHILD HAS THIS | AND ALSO THIS | HE MAY HAVE | |
| one or more painful joints |
|
 |
juvenile arthritis |
| other causes of joint pain See chart on joint pain. | |||
WALKS WITH DIFFICULTY OR LIMPS
| IF THE CHILD HAS THIS | AND ALSO THIS | HE MAY HAVE | ||
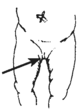
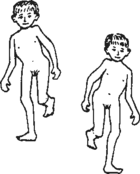
| dips to one side with each step | 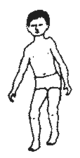 |
one leg often weaker and shorter |
Check for: | |
|
damaged hip joint | |||
| walks with knees pressed together |
|
spastic diplegic or paraplegic cerebral palsy | ||
 | ||||
| stands and walks with knees together and feet apart no other problems |
 |
feet less than 3” apart at age 3 | typical from ages 2 to 12 | |
 |
 |
feet more than 3” apart at age 3 | knock-kneed | |
| walks awkwardly with one foot tiptoe | muscle spasms and difficulty with control on that side. Hand on that side often affected. | hemiplegic cerebral palsy | ||
 |
(stroke in older persons) | |||
| walks awkwardly with knees bent and legs usually separated |
|
athetoid cerebral palsy | ||
 |
|
|||
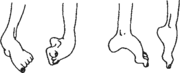
| walks with both feet tiptoe |
|
muscular dystrophy | ||
 |
legs and feet stiffen (spasticity of muscle) | spastic cerebral palsy | ||
| no other problems | typical? (some typical children at first walk on tiptoes) | |||
| walks with hand(s) pushing thigh(s) or with knee(s) bent back | 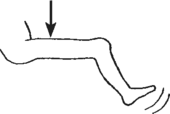
weak thigh muscle
difficulty lifting leg |
| ||
 | ||||
| Foot hangs down weakly (foot drop). | Child lifts foot high with each step so that it will not drag. | |||
| dips from side to side with each step | due to muscle weakness at side of hips, or double dislocated hips, or both |
| ||
 | ||||
| walks with one (or both) hip, knee, or ankle that stays bent | 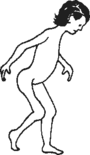 |
joints cannot be slowly straightened when child relaxes. |
| |
| Joints can gradually be straightened when child relaxes. | spasticity, often cerebral palsy | |||
| Knees wide apart when feet together (bow legs). Waddles or dips from side to side (if he walks). |
under 18 months old | often typical | ||
 |
Any combination of these:
|
Consider:
| ||
| flat feet |  |
no pain or other problems | normal in many children | |
|
may be problems in: | |||
BACK CURVES AND DEFORMITIES
| IF THE CHILD HAS THIS | AND ALSO THIS | HE MAY HAVE | ||
| sideways curve of backbone (scoliosis) |  |
When child bends over, look for a lump on one side. |  |
scoliosis—may occur alone or as complication of: |
 sway back (lordosis) |
|
lordosis—may occur in: | ||
| rounded back (kyphosis) |  |
kyphosis—often occurs with: | ||
| hard, sharp bend of or bump in backbone | 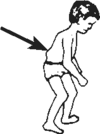 |
|
tuberculosis of the spine | |
| dark soft lump over backbone |  |
|
spina bifida (‘sack on the back’) | |
OTHER DEFORMITIES
| missing body parts | born that way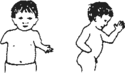 |
born with missing or incomplete parts | ||
| accidental or surgical loss of limbs (amputation) |  |
amputations | ||
| gradual loss of fingers, toes, hands, or feet, often in persons who lack feeling |  |
sometimes seen with:
| ||
| hand problems (For hand problems from birth, see "Activities to Help Develop Gripping, Reaching, and Hand‑Eye Coordination".) |
 |
may occur with:
| ||
 |
spastic cerebral palsy may lead to contractures | |||
| burn scars and deformities | burns | |||
| clubbing or bending of feet (For club feet from birth, see Chapter 11.) |
may begin as floppy weakness and become stiff from contractures, if not prevented |
may occur with many physical disabilities, including: | ||
 | ||||
DISABILITIES THAT OFTEN OCCUR WITH OR ARE SECONDARY TO OTHER DISABILITIES
| Developmental delay: child takes longer to learn to use her body or develop basic skills |
caused by slow or incomplete brain function or by severe physical disability, or both |
often seen in: |
 |
caused by overprotection: treating children like babies when they could do more for themselves | some delay can occur with almost any disability or lack of stimulation |
| Contractures joints that no longer straighten because muscles have shortened |
|
often secondary to: |
 Joints will not straighten. |
sometimes due to scarring from burns or injuries | burns |
| Behavior problems |
may come from:
|
behavior problems common with:
|
 | ||
| Slow to learn certain things; otherwise typical development. |
|
learning disability |
| Speech and communication problems |
|
may occur with: (Hearing loss may occur together with these and other disabilities.) |
 | ||
| other disabilities that sometimes occur secondary to other disabilities |
Main disability |
Common secondary disabilities |
| (Some of these we have already included in this chart.) |
|
|
|