Hesperian Health Guides
5. Skin problems
For all rashes, if the area of the rash is larger than your hand, or there are red streaks, fever, or any other serious signs with the rash, see a health worker.
Also see a health worker if a rash doesn’t respond to treatment.
Get medical help as soon as possible for any of these signs with rash:
- Pain in the bone behind the ear
- Headaches, dizziness, or a seizure
- Child is very tired or weak
- Hearing loss, deafness
Contents
Rashes with high fever
A number of different illnesses have signs that include some fever and skin rashes. But when a rash is combined with a high fever, it could be an illness spread by mosquitoes such as dengue.
Dengue usually begins with sudden high fever and chills, and body aches. After 3 or 4 days, the person begins to feel better for a few hours or days, then the illness returns for a few more days with a rash beginning on the hands and feet, and then spreading to the arms, legs, and body (but not the face). The headaches and physical pain that dengue brings can be very intense.
Signs of severe dengue — get medical help immediately!
- Bleeding from the skin
- Blood in vomit or feces (from stomach bleeding)
- The child is unable to eat or drink
- The child acts confused or loses consciousness
Rashes that itch
Many rashes are itchy. Tell children not to scratch the rash (and remind them when they forget), keep their fingernails trimmed, and wash their hands before bed and during the day to help prevent the rash from becoming infected.
Ways to help calm itchiness:
- Bathe rashy skin with cool water or, better yet, water in which oatmeal has been soaked.
- Leave skin rash open to the air when possible.
- Put calamine lotion or something to calm the itching on the rash several times a day.
- For severe itching, use 1% hydrocortisone cream on skin up to 4 times a day.
- An antihistamine medicine that contains diphenhydramine may help.
- Use paracetamol to treat pain from rashes.
Fungal rashes
Some itchy rashes are caused by fungus. The same fungus that causes thrush in a child’s mouth can also cause a scaly rash on the skin. Some fungal rashes are also known as “ringworm” although they are not caused by a worm. The rash may or may not itch, but is red, scaly, and has a raised edge and a pale center. These rashes may appear as diaper rash or on other areas of the torso, between toes or fingers, or on the face or scalp.
Treatment for fungal rashes
- Treat the skin several times a day with an antifungal cream containing clotrimazole, nystatin, or other similar medicines.
- Pills for fungal infections are hard on the liver and not recommended for children with HIV, but may be necessary to treat ringworm of the scalp.
Prevention of fungal rashes
- Keep feet and skin clean and dry.
- Wear sandals when washing in shared areas.
- Wash hands after touching pets or other animals, and don't sleep with animals.
- Don't share towels or other personal items.
Rashes that have blisters, sores, or pustules
If fluid-filled bumps appear and spread over the body and then form scabs after they burst, it could be chicken pox. Information about it and how to treat itching can be found in the previous section. But if the child has difficulty breathing, fever, or jaundice, see a health worker immediately.
Chicken pox (varicella)
Chicken pox is caused by a virus called varicella zoster. The child first gets a low fever and a rash of red, itchy spots which turn into fluid-filled, blistery bumps. They usually start on the child’s body and face, and then spread to her arms and legs. New itchy bumps may appear over a 5-day period and eventually burst and scab over. If scratched, bumps can get infected and turn into sores that take a long time to heal, and may leave scars. The infected rash can become very dangerous to a child with HIV. You can use the treatment for itchy rashes to make the child more comfortable, and give her extra fluids and nutrition.
Children with HIV that is not well controlled can develop pneumonia, meningitis and other srious problems. It the child has difficulty breathing, high fever, infected sores, jaundice, or a change in consciousness, see a health worker. Sometimes the medicine acyclovir (see below) is given to children with chicken pox.
Prevention of chicken pox
- Avoid contact with people who have chicken pox.
- The "live" chicken pox vaccine should not be given to children with untreated HIV. The "live" vaccine should only be given to children between birth and 5 years old who have CD4 counts of 500 or higher, and to children older than 5 with CD4 counts of 200 or higher.
Shingles (zoster)
The varicella zoster virus does not leave the body after the chicken pox goes away. It can stay hidden in the nerves and spine for months or years. Especially when a person is under a lot of stress, the virus can return. But instead of covering the whole body, the pustules are clustered in one area. This is called shingles, and can be very painful. It is often treated with acyclovir (see below).
Herpes (herpes simplex)
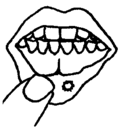
Herpes is a viral infection that causes blisters or ulcers on the lips (sometimes called a fever blister or cold sore). The first time a child gets herpes it may cause many blisters on the lips and in the mouth. After, herpes may cause either one or many sores or ulcers on the lips.
Give acetaminophen for pain, and use the same treatment recommended for other mouth sores. See a health worker for antiviral medicines if the sores return frequently or if the infection spreads near an eye — very dangerous!
For repeated herpes infections, severe chicken pox (varicella) or shingles (zoster).
GIVE
| Acyclovir: Give 15 mg for each kg, 5 times a day, for 7 days. Or dose by age: |
| Under 1 year old: give 100 mg (½ of a 200 mg capsule or ¼ of a 400 mg tablet), 5 times a day, for 5 days. |
| 1 to 3 years old: give 200 mg (a 200 mg capsule or ½ of a 400 mg tablet), 5 times a day, for 5 days. |
| 4 to 7 years old: give 400 mg (two 200 mg capsules or a 400 mg tablet), 5 times a day, for 5 days. |
Measles
Measles is caused by a virus and starts with a low fever, cough, runny eyes and nose, and sore throat (with white spots in the mouth). After 2 to 3 days, a red rash starts behind the ears, spreads to the neck and face, then the arms and body, and finally to the thighs, legs, and feet. Fever may rise to 40°C (105°F). The rash slowly fades, first from the face and last from the thighs and feet.
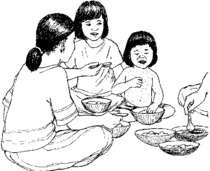
If a child with measles also develops diarrhea, give rehydration drink. For painful ear infection, difficulty breathing (pneumonia), or signs of meningitis, see a health worker. For children whose HIV is not well controlled, measles can be very dangerous.
Prevention of measles
- Avoid contact with people who have measles. Measles spreads very easily and can be dangerous for people with HIV and pregnant women.
- Do not give the "live" measles vaccine to children with untreated HIV. Children between birth and 5 years old should have a CD4 count of 500 or higher. Those older than 5 should have a CD4 count of 200 or higher.
Other skin bumps
Drug reactions
Blotchy, red, sometimes raised patches on the skin can be caused by an allergic reaction to a medicine. Usually the reaction begins soon after starting a new medicine. See a health worker as quickly as you can to change to a medicine that the child’s body can handle better.
Molluscum
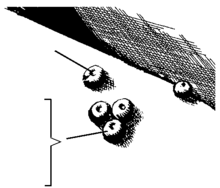
Round
Smooth
Painless
Molluscum is a skin condition caused by a virus that causes small bumps with a dimple in the middle and is usually white, pink or skin-colored. It usually starts as a small dot and grows over a week to the size of a small pea. It is common in children, especially children with HIV. It is not dangerous and will go away on its own after several weeks or months. It may go away after a child starts ART.
Prevention of molluscum
- Wash hands often with soap and water.
- Do not share towels, clothing, or other personal items.
- Do not touch or scratch bumps on your skin or other people's skin.
Warts or scaly red skin that does not itch
Warts or other bumps that do not itch can be left alone unless they become infected. Keep them clean and if they do not go away, ask a health worker if he knows how to remove them. Greasy and scaly red skin might be seborrhea, which can be treated with ketoconazole shampoo if there is hair, or 1% hydrocortisone cream 2 times a day on less hairy skin.


