Hesperian Health Guides
1. Diarrhea, dehydration, and vomiting
HealthWiki > Helping Children Live with HIV > Chapter 12: Common health problems > Diarrhea, dehydration, and vomiting
If there is blood in the diarrhea, the child needs medicine to get well.
Children with HIV often have diarrhea, and can get sicker from diarrhea than other children. For children with HIV, diarrhea leads more quickly to malnutrition and not gaining weight. Check a baby’s diapers for diarrhea. Ask older children to tell an adult if they have it.
The danger of diarrhea for any child is losing so much liquid that she becomes dehydrated, which can be deadly. One treatment is essential for everyone with any kind of diarrhea: drinking fluids to replace the liquid lost in the stools. Without drinking fluids, a child with diarrhea can lose so much fluid – become dehydrated – she can die. Even a child whose diarrhea is a side effect from starting ART needs more fluids.
Vomiting, like diarrhea, is a very visible sign. But just like diarrhea, it is less dangerous than dehydration. Learning how to make and give rehydration drink is a key to saving lives.
Contents
- 1 Dehydration
- 1.1 Signs of dehydration
- 1.2 General treatment for diarrhea, dehydration, and vomiting
- 1.3 Rehydration drinks
- 1.4 Rice water
- 1.5 Other home cereals
- 1.6 Yogurt or fermented milk drinks
- 1.7 What about plain water?
- 1.8 Must water be boiled?
- 1.9 Avoid drinks that make dehydration worse
- 1.10 Pre-packaged ORS
- 2 Treatment for diarrhea with other signs
- 3 Vomiting
Dehydration
Dehydration is a lack of water in the body. Children who become very dehydrated can die. The major cause of dehydration is untreated diarrhea, but fever, vomiting, or not being given enough fluids or breast milk can also cause it. Because dehydration from diarrhea or fever is so dangerous to young children, always be on the lookout for it, and be ready to give the child fluids.
Signs of dehydration
- Diarrhea, even if there are no other signs of dehydration
- Thirst, but children do not always say they are thirsty
- Dry mouth and tongue (the inside of the child’s cheek is dry)
- Urinating less often, and urine is dark-colored
Start giving fluids right away, before the signs get any worse.
Signs of severe dehydration
- Child is very tired and lacks energy
- Child’s heart beats very quickly
- Child breathes more deeply or gulps air
- Sunken, tearless eyes
- Sunken soft spot on baby's head
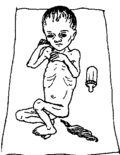
- Skin stays in a pinched shape when you pinch it
| Lift the skin on the child’s arm or stomach between your thumb and first finger. If the skin does not fall right back to normal, the child may be dehydrated. | 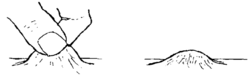 |
When dehydration becomes severe, the child is in serious danger. Quick treatment can save the child’s life.
Treatment for dehydration
The treatment for dehydration is simple: give fluids to drink that the body can absorb. See the recipes for rehydration drink below. If the child does not start to improve quickly, get help.
If you are breastfeeding, nurse more often — at least every 2 hours. Let the child breastfeed for as long as she wants. If the child is older than 6 months, also give rehydration drink, as much as the child will take after each feeding.
Rehydration drinks
Rehydration means replacing liquid the body loses during dehydration. Because diarrhea causes food to pass through too quickly, nutrients are lost, so rehydration should also replace nutrients. Water + a little salt + some energy food (sugar or rice or corn meal) = rehydration drink.
 |
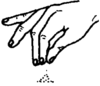 |  | |||
| 1 glass water | + | 1 pinch of salt | + | 2 or 3 teaspoons of sugar or cooked grain cereal |
After each stool, give as much rehydration drink as the child will drink. Each drink should be at least ¼ cup (2 ounces or 60 ml) for a baby, or a cup or more (8 ounces or 240 ml) for an older child or adult. Children may not feel like drinking a lot of fluid at once, so keep offering sips or spoonfuls, encouraging children to keep taking some in. Be patient.
Keep giving rehydration drink until diarrhea has stopped and signs of dehydration are gone.
Here are several ways you can prepare a good rehydration drink at home:
Salt and sugar drink, 2 ways:
This simple rehydration drink is just as good as the ORS (oral rehydration salts) packets you can buy
| 2 ways to make rehydration drink | |||||
| If you can, add half a cup of fruit juice, coconut water, or mashed ripe banana to either drink. These contain potassium, a mineral which helps a sick person accept more food and drink. | |||||
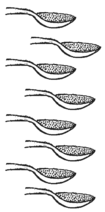
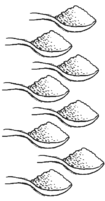
| 1. With sugar and salt. (You can use raw sugar or molasses instead of sugar.) | 2. With powdered cereal and salt. (Powdered rice is best. But you can use finely ground maize, wheat flour, sorghum, or cooked and mashed potatoes.) | ||||
| In 1 liter of clean WATER |
put half of a level teaspoon of SALT | and 8 level teaspoons of SUGAR | In 1 liter of clean WATER |
put half of a level teaspoon of SALT | and 8 heaping teaspoons of powdered CEREAL. |
 |
 |
 |
 | ||
| Boil for 5 to 7 minutes to form a liquid gruel or watery porridge. Cool the drink quickly and begin to give it to the sick person. | |||||
CAUTION! Before adding the sugar, taste the drink and be sure it is less salty than tears. |
CAUTION! Taste the drink each time before you give it to make sure that it has not spoiled. Cereal drinks can spoil within a few hours in hot weather. | ||||
Here are some other ways to rehydrate a child who has diarrhea.

Rice water
Cook some rice in twice as much water as you would normally use. Add about ½ teaspoon salt for a liter of water, or a big pinch for each cup of water. You can add a little sugar if you like. Have your child drink as much as she can. You can feed her the rice too.
Other home cereals
If you usually make porridge, pap or gruel to feed to young children, you can water it down to a thin liquid and add a little salt. Ground corn, dal, potato, or cassava will all work. But thinned porridge like this does not replace food. If you use thinned porridge for rehydration, also give regular, thick porridge to eat.
Yogurt or fermented milk drinks
These are good rehydration drinks and provide needed protein too. If the yogurt drink is very thick, add some water, and a pinch of salt.
What about plain water?
When a child is dehydrated, plain water is not as good as rehydration drinks because it lacks nutrients. But it is better to give plain water than nothing at all — for a little while. Give water while you wait for rice water or cereal drink to cook and cool, or another drink to be made.
Must water be boiled?
Water that has been boiled or disinfected is best. See more on how to make water safer to drink. But if you do not have a way to boil or disinfect water, use the water you do have until you can make your water safe.
Avoid drinks that make dehydration worse
Some drinks worsen dehydration, such as very sugary drinks, drinks with caffeine, and alcoholic drinks. So avoid:
- fizzy drinks (like Coke or Fanta, or beer).
- sugary fruit drinks.
- coffee and strong tea.
Pre-packaged ORS
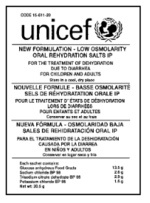
Packets of Oral Rehydration Salts (ORS, ORT) may be available from your pharmacy, clinic, or market. Like homemade rehydration drink, these are a mixture of salt and sugar. They also have potassium, citrate, and zinc, which are helpful nutrients for people with diarrhea. Where these packets are available for free, they are an easy way to make rehydration drink. Be sure to add the right amount of water — usually 1 liter of water per packet. (Check the instructions on the packet because adding too little or too much water can make the child worse.)
If ORS packets are not free, it is better, and much less expensive, to make your own rehydration drink. Your homemade drink is just as good as the drink made from the packet, and to recover from dehydration your child will need food as well as fluids. Spend your money on vegetables, beans, eggs, or other healthy foods, not on ORS packets.
Treatment for diarrhea with other signs
When a child has diarrhea along with other signs, such as fever or blood in the stool, he may need medicine in order to get well. Along with any medicine you give your child, be sure to give rehydration drink.
Diarrhea with blood or pus in stool
- Diarrhea with blood in it looks red, but sometimes blood may look black or very dark brown instead. Pus in diarrhea looks yellow.
- When there is blood in the stool but no fever, it is probably caused by dysentery.
- When there is blood in the stool and fever, it is probably caused by shigella or another bacterial infection.
Diarrhea with blood or pus, no fever: Dysentery
GIVE
| Metronidazole: Give 10 mg for each kg, 3 times a day, for 8 to 10 days. Or dose by age: |
| Under 3 years: give 62 mg (¼ of a 250 mg tablet), 3 times a day, for 8 to 10 days. |
| 3 to 7 years: give 125 mg (½ of a 250 mg tablet), 3 times a day, for 8 to 10 days. |
ALSO GIVE diloxanide OR ciprofloxacin.
| Diloxanide |
| Under 3 years: give 62 mg (⅛ of a 500 mg tablet), 3 times a day, for 10 days. |
| 3 to 7 years: give 125 mg (¼ of a 500 mg tablet), 3 times a day, for 10 days. |
| Ciprofloxacin |
| Under 3 years: give 125 mg (½ of a 250 mg tablet), 2 times a day, for 3 days. |
| 3 to 7 years: give 250 mg (one 250 mg tablet), 2 times a day, for 3 days. |
Diarrhea with blood or pus, with fever: Bacterial infection
It is difficult to know what medicine to use if you are not certain what infection is causing the child’s diarrhea, and also whether drug resistance in your area has changed which drugs will still work. Local health workers will know what are the most common infections and which antibiotic should work best.
Shigella is usually the most common infection, so treat for that. If the child is not better after 2 days, try one of the alternate medicines. Ask your local health worker. The first choice is azithromycin, but that may be expensive or not available, and you may be able to use one of the other medicines listed.
GIVE
| Azithromycin: Give 20 mg for each kg, one time only. Or dose by age: |
| Under 1 year: give 150 mg, one time only. |
| 1 to 3 years: give 250 mg, one time only. |
| 4 to 7 years: give 500 mg, one time only. |
OR GIVE
| Erythromycin: Give 10 mg for each kg, 4 times a day, for 3 days. Or dose by age: |
| Under 1 year: give 100 mg, 4 times a day, for 3 days |
| 1 to 3 years: give 150 mg, 4 times a day, for 3 days. |
| 4 to 7 years: give 200 mg, 4 times a day, for 3 days. |
OR GIVE
| Ampicillin: Give 10 to 25 mg for each kg, 4 times a day, for 7 days. Or dose by age: |
| Under 1 year: give 100 mg, 4 times a day, for 7 days. |
| 1 to 3 years: give 125 mg, 4 times a day, for 7 days. |
| 4 to 7 years: give 250 mg, 4 times a day, for 7 days. |
OR GIVE
| Cotrimoxozole (trimethoprim + sulfamethoxazole): Give 3 mg trimethoprim and 15 mg sulfamethoxazole for each kilogram, 2 times a day, until 3 days after signs have gone away. Or dose by age, using a single-strength 480 mg tablet (80 mg trimethoprim and 400 mg sulfamethoxazole): |
| 6 weeks to 12 months: give ¼ tablet (20 mg trimethoprim and 100 mg sulfamethoxazole), 2 times a day, until 3 days after signs have gone away. |
| 1 to 3 years: give ½ tablet (40 mg trimethoprim and 200 mg sulfamethoxazole), 2 times a day, until 3 days after signs have gone away. |
| 4 years to 7 years: give 1 tablet (80 mg trimethoprim and 400 mg sulfamethoxazole), 2 times a day, until 3 days after signs have gone away. |
| Note: If the child already takes cotrimoxazole, add another medicine from this section. Continue to give the child their usual dose of cotrimoxazole. |
In some places resistance to these medicines has developed. This means they no longer work and ceftriaxone should be used instead. See a health worker to get an injection of the correct amount.
Diarrhea is yellow and bubbly: Giardia
GIVE
| Metronidazole works best. Dose by weight and give for 5 days. For a child under 3 years old: give 8 to 15 mg for each kg, 2 times a day. For a child from 3 to 7 years old: give 12 to 16 mg for each kg, 3 times a day. Or dose by age: |
| Under 3 years: give 62 mg (¼ of a 250 mg tablet), 2 times a day, for 5 days. |
| 3 to 7 years: give 62 mg (¼ of a 250 mg tablet), 3 times a day, for 5 day. |
OR GIVE
| Quinacrine can also be used and may be cheaper. Give 2 mg for each kg, 3 times a day, for 1 week. Or dose by age: |
| Under 10 years: give 50 mg, 3 times a day, for 1 week. |
Diarrhea with vomiting
This could be caused by: a virus, or unclean water or food. So long as you treat with rehydration drink, the child should get better.
Diarrhea with vomiting and and fever
This could be caused by different viruses, or it could be cholera – a health worker will know if there is chlolera in the region. Always give rehydration drink too.
Treatment for cholera
GIVE
| Azithromycin: Give 20 mg for each kg, one time only. Or dose by age: |
| Under 1 year: give 150 mg, one time only. |
| 1 to 3 years: give 250 mg, one time only. |
| 4 to 7 years: give 500 mg, one time only. |
OR GIVE
| Erythromycin: Give 10 mg for each kg, 4 times a day, for 3 days. Or dose by age: |
| Under 1 year: give 100 mg, 4 times a day, for 3 days. |
| 1 to 3 years: give 150 mg, 4 times a day, for 3 days. |
| 4 to 7 years: give 200 mg, 4 times a day, for 3 days. |
Tetracycline, doxycycline, and ciprofloxacin also work for cholera, but they are not recommended for children younger than 8 years old. But because cholera is such a dangerous illness, use one of these medicines if that is all you have.
Vomiting
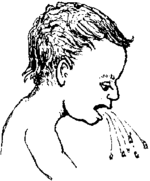
Usually vomiting is caused by a virus, and will pass. Too much vomiting can cause dehydration, so give fluids and watch for dehydration].
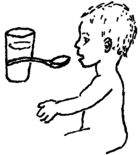
If a child vomits more than once in an hour, or shows signs of dehydration, give rehydration drink. At first, give just a spoonful every 15 minutes, even if he continues to vomit. If the drink stays down, give a spoonful every 5 minutes. Then give larger sips. You can also use other liquids.
Giving more fluids and food as soon as possible will help the child regain his strength. Children may not want to drink anything while they are feeling nauseous. Encourage them to sip small amounts as often as possible.
If a child vomits blood, or vomits every few minutes for 3 hours, or cannot keep down any rehydration drink, get medical help.
When a child vomits within 20 minutes after taking medicine, the medicine may be vomited too. Wait until vomiting has stopped before you give more medicine. As soon as a child is rehydrated and drinking, you can give medicine as usual. For children with HIV who must take ART regularly, see Side effects while taking ART.
Some children are very upset by vomiting or may have stomach pains. Reassure children that it will stop soon, and help them rest.