Hesperian Health Guides
Questions in a pregnancy health history
HealthWiki > A Book for Midwives > Chapter 7: Learning a pregnant woman's health history > Questions in a pregnancy health history
Contents
- 1 Does she have signs of pregnancy?
- 2 How pregnant is she now? When is the baby due?
- 3 How old is she?
- 4 How many children has she had?
- 5 Has she had any miscarriages or abortions?
- 6 Has she had any problems with past pregnancies or births?
- 6.1 Was she tired or weak (anemic)?
- 6.2 Did she have high blood pressure?
- 6.3 Did she have pre-eclampsia?
- 6.4 Did she have convulsions?
- 6.5 Did she have diabetes (blood sugar disease)?
- 6.6 Did she have a very long labor or a long pushing stage?
- 6.7 Did she have a fistula?
- 6.8 Did she have a very short labor (less than 3 hours)?
- 6.9 Did she have an early birth?
- 6.10 Did she have a small baby (less than 2.5 kilograms or 5 pounds)?
- 6.11 Did she have a big baby (over 4 kilograms or 9 pounds)?
- 6.12 Did she have heavy bleeding before or after the birth?
- 6.13 Did she have any problems with the placenta?
- 6.14 Did she have a fever or infection of the womb during or after the birth?
- 6.15 Was she very sad (depressed) after the birth?
- 6.16 Did the baby get sick or die before, during, or after the birth?
- 6.17 Did her baby have disabilities at birth?
- 6.18 Did she have a cesarean surgery (birth by operation)?
- 7 Is she healthy?
- 8 Has she been vaccinated against tetanus? If yes, when?
- 9 Is she taking any medicines now?
- 10 Has any medicine ever given her problems?
- 11 What else in her life might affect her pregnancy and birth?
Does she have signs of pregnancy?
Some signs of pregnancy are sure signs — they mean the woman is definitely pregnant. Some signs are probable signs, meaning the woman is probably pregnant, but the sign could be caused by something else.
Probable signs of pregnancy
The woman’s monthly bleeding stops. This is often the first sign of pregnancy. Other possible causes of this sign are poor nutrition, emotional troubles, or menopause (change of life).
The woman has nausea or wants to vomit. Many pregnant women have nausea in the morning (which is why this feeling is often called “morning sickness”), but some women may feel this way all day. Nausea is common during the first 3 months of pregnancy. Other possible causes of this sign are illness or parasites.
The woman feels tired and sleepy during the day. This is common in the first 3 or 4 months of pregnancy. Other possible causes of this sign are anemia, poor nutrition, emotional troubles, or too much work.
The woman needs to urinate often. This is most common during the first 3 months and the last 1 or 2 months of pregnancy. Other possible causes of this sign are stress, bladder infection, or diabetes (blood sugar disease).
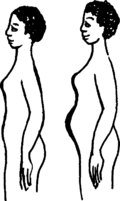
The woman’s belly grows. After 3 or 4 months, the pregnancy is usually big enough to be seen from the outside. Other possible causes of this sign are that the woman has a cancer or another growth in her belly or that she is just getting fatter.
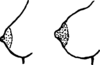
The woman’s breasts get bigger. A pregnant woman’s breasts get bigger to prepare to make milk for the baby. Another possible cause of this sign is that breasts often get bigger just before monthly bleeding.
The woman feels light baby movements inside. Most women start to feel their babies move between about 16 weeks and 20 weeks of pregnancy (at about 4 or 5 months). Another possible cause of this sign is gas in the belly.
Sure signs of pregnancy
The woman feels strong baby movements inside. Most women begin to feel the baby kicking by the time they are 5 months pregnant.
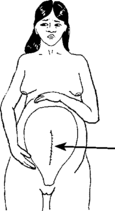
The baby can be felt inside the womb. By the 6th or 7th month, a skilled midwife can usually find the baby’s head, neck, back, arms, bottom, and legs by feeling the mother’s belly.
The baby’s heartbeat can be heard. By the 5th or 6th month, the heartbeat can sometimes be heard with tools made for listening, like a stethoscope or fetoscope. By the 7th or 8th month, a skilled midwife can usually hear the baby’s heartbeat when she puts her ear on the woman’s belly.
A medical pregnancy test says the woman is pregnant. This test can be done with a kit at home or in a laboratory with a little of the woman’s urine or blood. This test can be expensive and is usually not necessary. But it can be useful, for example, if a woman needs to know if she is pregnant before taking a medicine that might harm a baby inside her.
How pregnant is she now? When is the baby due?
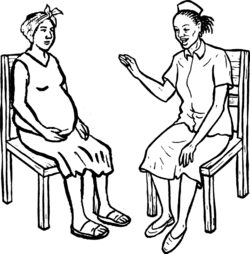
Find out how many months pregnant the woman is at the time of her first checkup. This will help you estimate about when she will give birth (the "due date").
There are 3 ways to figure out how pregnant the woman is now and her due date:
- Use the date of her last monthly bleeding.
- Measure the size of her womb.
- Have the woman get an ultrasound at a medical center.
date and 2 weeks after it.
Using the last monthly bleeding to predict the due date
If a woman bleeds regularly every 4 weeks, her pregnancy will start about 2 weeks after the first day of her last monthly bleeding. To find out if you can use this method to estimate her due date, you must first ask the mother 3 questions:
- Has your monthly bleeding been mostly regular, once every 4 weeks (once every month)?
- Was your last monthly bleeding normal for you (not unusually light or heavy)?
- Do you remember the date of the first day of your last monthly bleeding?
If the woman answers “no” to any of these 3 questions, you cannot be certain this method will give you a correct due date.
If she answers “yes” to all 3 questions, you can figure out the due date and how pregnant the woman is at this visit.
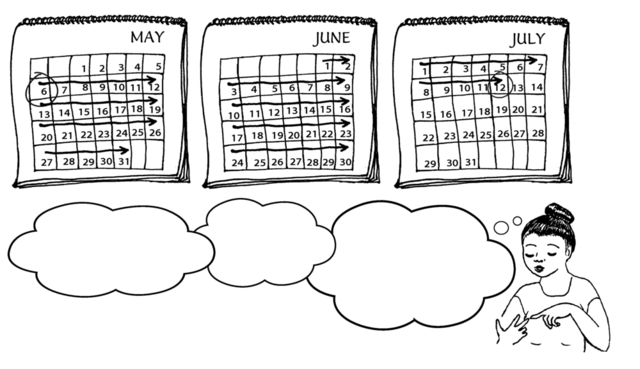
Remember that a pregnancy lasts about 40 weeks or 280 days. This is about 9 calendar months or 10 lunar months from the last monthly bleeding.
Using a calendar
To figure out the due date, add 9 months and 7 days to the day that her last monthly bleeding began.
(You could also subtract 3 months and then add 7 days to get the same date.)
See a helpful tool to estimate the due date using the last monthly bleeding.
To figure out how pregnant the woman is now, take the first day of the last monthly bleeding and count the number of weeks that have passed between that day and this visit.
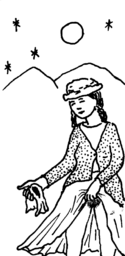
Using the moon
If you do not use calendars, you can find the due date using the moon. If a woman’s monthly bleeding is usually about one moon (4 weeks) apart, the baby is due 10 moons after the first day of her last monthly bleeding. If a woman’s monthly bleeding started on a quarter moon, the baby is due 10 quarter moons later. If her bleeding started on a new moon, the baby is due 10 new moons later, and so on.
For example:
 |
 |
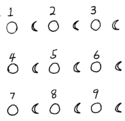 |
 |
| If her bleeding started on the full moon, | she probably got pregnant on the new moon. | The baby is due 10 lunar months after the first day of her last monthly bleeding — | in this case, 10 full moons after the first day of her last monthly bleeding. |
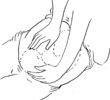
Measuring the womb
With practice, a midwife can feel the size of the woman’s womb to know how long a woman has been pregnant. Use this method when:
- the woman does not remember when her last monthly
bleeding started. - the last monthly bleeding was unusually light or heavy.
- her monthly bleeding is not regular.
- the woman was breastfeeding and not bleeding regularly
when she got pregnant.
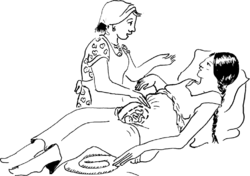
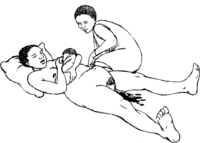
There are two ways to measure the womb. During the first 12 weeks (3 months) of pregnancy you can do a bimanual exam to feel the womb from inside the vagina. After 3 months you can measure the womb from the outside.
Using a sonogram
A sonogram (or ultrasound) machine takes a picture of the baby inside the womb by using sound waves. A sonogram done in the first 6 months of pregnancy is an accurate tool for showing how far along the pregnancy is and if there are any problems. Sonograms are not dangerous for the baby
How old is she?
Pregnancy can cause problems for women of any age. But very young women and much older women tend to have more problems.

Girls who become pregnant before they are 17 years old may not have finished growing themselves. A girl’s pelvis might not be grown enough to give birth safely. Girls are more likely to have other problems too — like pre-eclampsia, long labors, and babies born too early. Girls who get pregnant when they are very young can be wonderful and caring mothers, but many of them will need extra advice and support.
Older mothers also may have more problems in pregnancy and birth.
It may be safer for older women and very young women to give birth in a well-equipped medical center rather than at home.
How many children has she had?
Women who have had 1 or 2 babies and whose children were born alive and healthy usually have the fewest problems giving birth.
Other women may have more problems. First births are often more difficult than later births. It may be safer for a woman giving birth for the first time to give birth near a medical center. Watch carefully for risk signs and have transportation available for emergencies.
A woman who has given birth to 5 or more babies is more likely to have some of the following problems:
- a long labor
- a torn womb (after a long, hard labor)
- a fallen womb (prolapsed uterus)
- a baby in a difficult position for birth
- heavy bleeding after birth
For these reasons, it may be safer for a woman who has had 5 or more births to give birth in or near a medical center.
Has she had any miscarriages or abortions?
Miscarriage
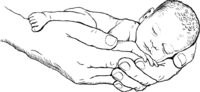
A miscarriage (spontaneous abortion) is when a pregnancy ends early because the developing baby dies for some reason. Most miscarriages happen in the first 3 or 4 months, often before the woman knows she is pregnant. After 5 or 6 months, a miscarriage is sometimes called a “stillbirth.” Some babies born before they can live outside the mother may survive in a well-equipped hospital.
It is usually difficult to know why a miscarriage happens, but some causes of miscarriage are preventable. Malaria, sexually transmitted infections, injury, violence, and stress can all cause a pregnancy to end.
Sometimes miscarriages happen because a woman has been near poisons or toxic chemicals. For example, women who work on farms often breathe or handle pesticides which can cause miscarriage.
Some miscarriages can be prevented by treating women for illness and infection and by helping them avoid chemical poisons and violence. But some women have one miscarriage after another, and you may not know why. Get medical advice to find the cause and to help her carry this pregnancy all the way through.
Abortion
Many women use plant medicines and other remedies to regulate or bring on their monthly bleeding, or prevent or end a pregnancy. These remedies may be safe, but ask the woman if she has ever had a problem — such as pain, heavy bleeding, or infection — after using any plant or any kind of medicine.
When a person, or the woman herself, does something to to end a pregnancy, this is called an abortion. There are several ways to have a very safe abortion, especially in places where abortion is legal, available, affordable, and a woman can see a health worker if she has any problems. Safe abortion methods include:
- Medication abortion. The woman takes medicines that end the pregnancy and empty the womb. The medicines used most often are misoprostol, used either by itself or with mifepristone. Learn how these drugs can be used safely.
- Vacuum aspiration. A health worker uses a machine or manual vacuum aspiration (MVA) syringe to create suction that empties the womb (see Chapter 23). When vacuum aspiration is done under clean conditions by a trained health worker using the proper instruments, it is very safe.
- D&E (dilation and evacuation). A health worker uses a combination of suction and sterile medical instruments to empty the womb. This should only be done by a trained medical worker.
In places where abortion is illegal, women may use methods that are unsafe or not effective when trying to end pregnancies. Unsafe abortions can cause heavy bleeding, serious infection, infertility, or even death. See Chapter 22 to learn how to help a woman after an unsafe abortion.
A woman who was sick, injured, or bled heavily after any kind of abortion may have scars in her womb that could cause problems in this pregnancy or birth. It is probably safest for her to give birth in or near a hospital or medical center.
Has she had any problems with past pregnancies or births?
If a woman has had problems with past pregnancies or births, she may have problems with this birth too.
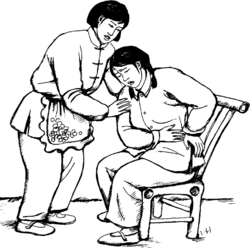
Ask the mother to tell you the story of each of her past pregnancies and births. Let her tell you everything: the good and the bad. Then ask the following questions to learn more about problems in past pregnancies and what to be prepared for during this one. If you can, write down what you learn. (Many of these problems are explained more fully in other parts of this book. Click on the link to learn more about the problem.)
Was she tired or weak (anemic)?
Extreme tiredness or weakness in pregnancy is usually caused by anemia (lack of iron in the blood). If she had anemia in another pregnancy, she is likely to have it again in this pregnancy. Anemia causes problems in pregnancy and birth, but it can be prevented by eating lots of foods with protein and iron in them and by taking iron pills. Women with anemia are often also at risk for pre-eclampsia.
Did she have high blood pressure?
If she had high blood pressure in a past pregnancy, she is likely to get it again. High blood pressure can be a sign of pre-eclampsia.
Did she have pre-eclampsia?
If a woman had pre-eclampsia in a past pregnancy, she is in danger of getting pre-eclampsia again. Check her blood pressure and other signs of pre-eclampsia regularly in this pregnancy. Be prepared to get medical help if pre-eclampsia develops.
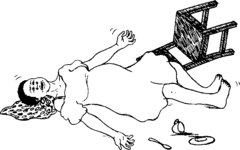
Did she have convulsions?
If she had convulsions in a past pregnancy or birth, get medical advice. She probably had eclampsia. She is likely to get it again, and she should give birth in a medical center or hospital.
Did she have diabetes (blood sugar disease)?
If she had diabetes in a past pregnancy, she is more likely to get it again. If possible, she should be tested by a doctor or health worker. Diabetes in the mother can lead to miscarriage or other problems with the mother or baby after birth.
Did she have a very long labor or a long pushing stage?
Was her labor longer than 24 hours for a first baby, or longer than 12 hours other babies? Did she push for more than 2 hours? Ask if her long labor caused problems for her or her baby. If that birth was healthy and the baby was OK, then she will probably not have a problem with this birth. If that birth was long, ask her if she knows why. Did she have anemia? Was the baby in a difficult position or very big? Was she very afraid? You may need to get medical advice.
Did she have a fistula?
If she had a long labor leading to a fistula (an opening in the tissue of the vagina) she should have this birth in a hospital.
Did she have a very short labor (less than 3 hours)?
If the mother had a very short labor in the past, make sure she and her family know what to do if you do not get there in time. You can teach the family how to deliver a baby in an emergency.
Did she have an early birth?
If she had a baby born more than a month early, ask her if she has signs of bacterial vaginosis (BV). Bacterial vaginosis can lead to early births. Be ready in case this baby is early too, and watch for signs of labor.
Did she have a small baby (less than 2.5 kilograms or 5 pounds)?
Find out if the baby was born early (it is not unusual for early babies to be small). If the baby came on time, ask the mother if she had anemia, high blood pressure, or pre-eclampsia. Also ask if she had enough to eat, or if she smoked cigarettes or used drugs. Any of these things could have made the baby small.
Check to see if this baby is growing well. If you think this baby may be very small for her age, the mother should probably give birth in or near a medical center, because small babies can have more health problems.
Did she have a big baby (over 4 kilograms or 9 pounds)?
Ask if the birth was difficult. If it was not, this birth will probably be OK too. Look for signs of diabetes. Check carefully to see if this baby seems big too. If possible, have the mother tested for diabetes.
Did she have heavy bleeding before or after the birth?
If she bled a lot in a past pregnancy or birth, it is likely to happen again. Ask her to tell you as much as she can remember about her bleeding. Did she need medical help? Was she anemic? Was she too weak to stand? The answers to these questions will help you prepare for what may happen at this birth. If possible, a woman who bled heavily before should have her babies in a medical center. Be ready to treat her for heavy bleeding after the birth.
Did she have any problems with the placenta?
If the woman’s placenta did not come out easily in a past birth, she may have the same problem again. Be ready to treat her for bleeding. It is better if she gives birth in or near a medical center.
Did she have a fever or infection of the womb during or
after the birth?
This birth may be fine, but she has more risk of infection than other women. Be sure to check her for signs of infections that are spread mainly through sex (see Chapter 18).
Was she very sad (depressed) after the birth?
If a woman became depressed after a past birth, it may happen again. Be prepared to help if this happens.
Did the baby get sick or die before, during, or after the birth?
Find out if the baby was sick or died. If some of her babies died, she may have a problem in her blood called Rh incompatibility. Or the deaths could have had other causes. Check the mother for high blood pressure, diabetes, anemia, malnutrition, and illness. These can all cause death in babies. Get medical advice.
Did her baby have disabilities at birth?
- Some disabilities run in the family. Ask about the type of disability and if anyone else in her or the baby’s father’s family has had that. The next baby may have the same problem.
- Some disabilities are caused by illnesses like German measles (rubella) during pregnancy. Pregnant women should avoid people who are sick. If the woman had rubella in a past pregnancy, it probably will not cause disabilities in the baby in this pregnancy.
- Some disabilities are caused by exposure to toxic chemicals, drugs, or medicines during pregnancy.
- Some disabilities are caused by poor nutrition during pregnancy.
- Some disabilities just happen — no one knows why.
Learn more about disabilities present at birth.
Did she have a cesarean surgery (birth by operation)?
In a cesarean surgery, a doctor cuts open the woman’s belly and womb to get the baby out. After the baby is out, the doctor sews the womb and belly closed. This leaves one scar on the womb and a second scar on the belly. Sometimes a cesarean surgery is done because the baby does not fit through the mother’s pelvis. Sometimes it is done because the baby is in danger and must be born very quickly.
Most women can have a safe vaginal birth even if they had a cesarean with a previous baby. But there is a very small chance that the scar on the womb may tear open during labor. If this happens, the woman could bleed inside and she or the baby could die. For this reason, it is safest for a woman who has had a cesarean to give birth in or near a medical center or hospital. If she is planning to give birth at home, arrange for her to have medical care in case there are any problems during the labor.
If any of the following are true, this woman should definitely go to a medical center for the birth:
 |
 A scar on the womb that goes this way is more likely to open up in labor. |
| A scar that goes one way on the outside... |
...may be hiding a scar on the womb that goes another way. |
- The cesarean was less than 2 years ago.
- This baby is big or in a difficult birth position.
- The woman had a cesarean
because her pelvis was not formed well as a child. This is usually caused by poor nutrition. - The scar on the womb is up-and-down.
Unfortunately, you cannot tell anything about the scar on the womb by looking at the belly. The scar on the belly can be one way, and the scar on the womb inside can be another. You can only find out by checking the medical records at the hospital or by asking the doctor who did the surgery.
Is she healthy?
A pregnancy is more likely to go well for a woman who is in good health. See Chapter 4 for general ideas for staying healthy. Also see Chapter 18 to learn about avoiding infections that spread mainly through sex. Some general health problems can cause serious problems in pregnancy.
Ask if she uses tobacco, alcohol, or other substances or works with chemicals.
If a pregnant woman has, or might have, any of the following, she should have help planning for her needs during pregnancy, getting testing and treatment (if appropriate), and deciding if it is safer to give birth in a medical center:
- depression
- drug or alcohol use
- diabetes
- HIV
- bladder or kidney infection
- malaria
- fever over 38°C (100.4°F) for more than 2 days
- any sexually transmitted infections (STIs), especially syphillis or gonorrhea
- high blood pressure
- liver disease (hepatitis, especially hepatitis B)
- heart problems
- tuberculosis
- deformity of the hips or lower back
Malaria
Malaria is an infection of the blood spread by mosquitoes. Malaria causes chills and fever. Malaria is especially dangerous for pregnant women and their babies. Malaria in pregnancy can cause anemia, miscarriage, early birth, small baby, stillbirth (baby born dead), or dangerous problems like eclampsia or bleeding.
Pregnant women should avoid malaria (see below) and be treated quickly if they get sick. Malaria medicines may be costly and can have side effects, but these medicines are much safer than becoming sick with malaria. Use a malaria rapid test to know who needs treatment.
For severe malaria, anyone who is pregnant needs emergency treatment in a hospital or clinic with the same medicines used for any other adult. Signs of severe malaria include: mental confusion or convulsions, difficulty staying awake, repeated vomiting, difficulty or rapid breathing, and being too weak to sit or stand.
With regular (uncomplicated) malaria, treating right away is important so that it does not get worse. After the first 3 months of pregnancy, the treatment for malaria is the same as for any other adult in your region. In most countries, ACT (artemisinin-based combination therapy) will be used. There are many types of ACT and malaria treatment is not the same everywhere, so find out from the local health authority which medicines work where you live. Common ACT combinations are listed below.
For uncomplicated malaria during the first 3 months of pregnancy: give 600 mg of quinine by mouth, 3 times a day for 7 days AND give 300 mg of clindamycin by mouth, 4 times a day for 7 days. If a test shows vivax malaria, or if you do not have clindamycin, use only quinine. If you cannot get those medicines, you can give ACT any time during pregnancy.
Common ACT medicines to treat malaria include:
- artemether + lumefantrine
- artesunate + amodiaquine
- artesunate + pyronaridine
- artesunate with sulfadoxine + pyrimethamine
- dihydroartemisinin + piperaquine
Quinine, chloroquine, clindamycin, and proguanil are all safe during pregnancy. Primaquine is not safe to use during pregnancy.
Pregnant women who live where there is a lot of malaria can use sulfadoxine-pyrimethamine to prevent it. Do not use during the first 3 months of pregnancy, but after that give at least 3 times during pregnancy with at least 1 month between treatments. Do not give more than 0.4 mg folic acid a day while giving sulfadoxine-pyrimethamine, as higher doses of folic acid make the medicine less effective. Do not give to people who are HIV-positive and taking cotrimoxazole.
To prevent malaria, avoid mosquito bites and control mosquitoes.
- Sleep under treated bed nets or hang treated curtains in doors and windows, especially if you are pregnant. Treated bed nets are safe, but do not spray pesticides on bedding.
- Get rid of standing water and stay away from wet places where mosquitoes breed.
- Give children the falciparum malaria vaccine now being used in high malaria areas.
- Use citronella oil or mosquito repellent on skin when mosquitoes are biting.
- Create community programs to destroy mosquitoes without using strong chemicals.
HIV
HIV is a virus that weakens a person’s immune system so they cannot fight illness. Ongoing treatment with medicines (called ART) can control it so a person with HIV can live a healthy life and not spread HIV to others. Without treatment, a person with HIV may seem healthy for years, but will become ill more often and more seriously, and eventually will develop AIDS and die. Medicines and good nutrition are both important to stay healthy with HIV. See more about HIV.
Prevent HIV during pregnancy
It is impossible to know by looking at someone whether they have HIV. Without an HIV test, most people do not know they have HIV until they are very sick. Even if they are not sick, their HIV can spread at any time. Encourage anyone who is pregnant, as well as others in their family (including partners and children), to be tested for HIV. Get people on treatment quickly if needed. HIV can spread to a baby during pregnancy, birth, or breastfeeding if the mother has HIV and is not using ART medicines.
If a woman's partner has HIV or will not get tested, and the woman does not have HIV, she can take ART medicines to prevent becoming infected (called pre-exposure prophylaxis, or PrEP). PrEP also protects the developing baby during pregnancy, birth, and breastfeeding. Using condoms also protects against HIV and other sexually transmitted infections. See STIs that affect the whole body.
Care for pregnant women with HIV
Give a pregnant woman with HIV the same respect and care you would give any woman. If they are using ART, the medicines that fight HIV, women with HIV can safely be pregnant and have healthy babies.
Note: Some women first find out they have HIV when they are tested during pregnancy. These women need support to cope with this news and what it may mean for their families. Health workers and midwives should take care not to discuss a woman’s HIV status with anyone (including each other) without her knowledge and consent.
Pregnant women with HIV need to take even more care with their health than others. Eating well, avoiding infections, and treating illness quickly are most important. Encourage a pregnant woman with HIV to start ART treatment right away, and if possible, join a support group with other pregnant women with HIV. Help her to get enough food if this is a problem. Explain why she should see you or another health worker regularly, and help her identify where to get good medical care nearby in case she needs it If there is a well-equipped medical center in your area, it might be better for her to give birth there.
Watch women with HIV for signs of other sexually transmitted infections, especially syphilis (see Chapter 18). Help them prevent malaria and get tested for TB (tuberculosis) and hepatitis. Help women (and their partners) get treatment for these or other infections.
A woman with HIV can prevent many infections (pneumonia, diarrhea, malaria, and others) by taking a low-cost antibiotic called cotrimoxazole every day.
ART Medicines to protect developing babies
Without treatment, about 1 out of 4 babies born to women with HIV is infected with HIV at birth. With treatment, the risk is 1 out of 50. The baby will also need to take ART medicines after birth.
See more about these uses of ART. (Also learn about preventing the spread of HIV while breastfeeding).
Other problems to watch for
Besides making infections harder to fight, HIV can also cause:
- loss of pregnancy, especially late in pregnancy (stillbirth)
- early birth
- bleeding and infection after birth
Try to be prepared for any of these if caring for a pregnant woman with HIV. To learn more about supporting women with HIV and their children, see Hesperian's Helping Children Live with HIV.
Midwives can help stop HIV
Midwives can help stop HIV by teaching others in their community how HIV spreads and how treatment both keeps people with HIV healthy and stops it from spreading. Help people get tested and get the ART medicines they need. With treatment, HIV is a manageable illness, but preventing it is still important. To protect babies, help women who have HIV plan carefully for pregnancy, and prevent pregnancies they do not want (see Chapter 17). Help women who are pregnant or breastfeeding avoid becoming infected with HIV. New HIV infections during pregnancy are more likely to spread HIV to the baby too.
Work with others in your community to teach people about safer sex and the benefits of using condoms. Find ways to help people talk about HIV, get tested, disclose their status to partners, and ask others to use condoms. Encourage people who are comfortable doing so to speak with others.
One way to help prevent HIV is to teach people about using condoms. But even when people know how condoms protect them from HIV, they often need support to use this knowledge. For example:
- Some people, especially many young people and women, cannot choose how they have sex. If they do not want sex, or they want to use condoms, their partners may not agree.
- Some people do not want to use condoms. Other people cannot afford to buy condoms, or cannot find them easily.
- Some people just feel hopeless, especially if life in general is very hard and many people around them are struggling.
These challenges are not easily solved. Find ways to talk to people and to encourage them to talk to each other about HIV, about why people have difficulty protecting themselves from HIV, and how to change this.
Has she been vaccinated against tetanus? If yes, when?
Tetanus (lockjaw) is caused when a germ that usually lives in dirt or stool enters the body through a wound. A woman can get tetanus if something that is not sterile is put into her womb or vagina during or after childbirth or from an unsafe abortion. A baby can get tetanus if the cord is cut with something that is not sterilized, or when anything (like dirt or dung) is put on the cord stump.
Tetanus vaccinations
Everyone should get a series of vaccinations to prevent tetanus (lockjaw). Every country has its own schedule of when to give them and which vaccines are given together. In general, a child gets 3 injections during the first year of life, and three more (called “boosters”) afterwards. The combination vaccines have names including DPT, Tdap, Dt, DTaP, and others. It is best if these vaccinations happen early in life to prevent ever getting sick with tetanus. If someone did not get all 6 injections, and has not had an anti-tetanus vaccination in the past 10 years, they need a “booster” now to be protected.
People who have received all the 6 vaccinations will not get sick if they are exposed to tetanus.
If the mother has not received all the vaccination doses, give a dose of anti-tetanus vaccine when you begin seeing her. Give another dose at least 4 weeks later, and at least 2 weeks before she gives birth. The baby will not be protected by only 1 dose of the vaccine.
If the woman cannot remember if she has had the vaccination or not, assume that she has not and give her the vaccinations. Extra doses will not harm her.
Vaccinations during pregnancy will also protect the baby from tetanus during the first few weeks after birth. But the baby must be vaccinated after birth so that the protection will continue.
Has she been vaccinated against COVID 19?
COVID 19 is a virus that makes some people very sick, though others get only mild illness. There is an increased risk of serious illness from COVID 19 during pregnancy, which is dangerous for both the mother and the baby.
COVID 19 vaccines prevent death and serious illness, and are safe during pregnancy and breastfeeding.
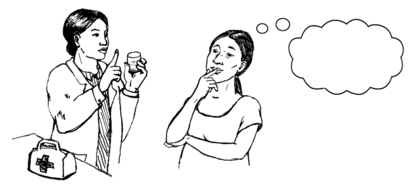
Is she taking any medicines now?
It is best for a woman to avoid most modern medicines and plant medicines during pregnancy. Many medicines can harm the baby inside the womb.
If a woman needs to take a medicine, see the Medicines Pages of this book to find out whether that medicine is listed as safe in pregnancy. If the medicine is not listed, get medical advice.
Supplements and tonics
Some modern and plant medicines that are not dangerous are called supplements or tonics. Prenatal vitamins and iron pills are healthy and safe supplements. They help the body get the vitamins and minerals it needs.
Some plants are not used to heal sickness, but to make the body stronger. These herbs have vitamins and minerals that help the baby grow. They are safe and helpful in pregnancy. Some of these tonic plants are nettles, alfalfa, and red raspberry leaf. These plants have different names around the world, so ask someone experienced with plant medicines before giving any tonic herbs to pregnant women.
Has any medicine ever given her problems?
If the woman has ever had a health problem after taking a medicine, like a rash, swelling, or difficulty breathing, do not give her that medicine. Those problems are signs of allergy. If a woman takes a medicine that she is allergic to, she might become very sick or even die. An allergic reaction can happen at any time during the rest of her life.
Write down the name of the medicine so you can both remember it. Explain to the woman that she must never use the medicine again, and that she should always tell her doctors or health workers what happened when she used the medicine.
Medicines that are not in the same family as the one she is allergic to are as safe for her as for
anyone else.
What else in her life might affect her pregnancy and birth?
Money
Not having enough money causes many problems for pregnant women. Eating poorly during pregnancy is dangerous for both the mother and the baby. Money worries add to stress, fear, and sadness, which can make the pregnancy and any other health problems more difficult. Lack of money may limit options if emergency care is needed.
If the woman you are helping cannot afford enough food to be healthy, help her find resources in the community. Religious groups or mother and child health programs may have food assistance they can provide, such as powdered milk, dried beans, grains, and cooking oil.
Living conditions
- Is there a clean and private place she can give birth?
- Is clean water available?
- Does anyone in her house have a serious disease that she might catch (contagious disease)?
- Does anyone smoke cigarettes in the house? Is there a smoky cooking stove inside the house? Both kinds of smoke are very harmful.
Help her find a clean, safe place to give birth.
Distance from care
- Will she be able to come to her pregnancy checkups? Can you go to her?
- If she lives far away, can you teach her to do some of the pregnancy checkup herself?
- How far is the maternity center, clinic, or hospital? Does she need to stay nearby at the end of her pregnancy to be closer?
- How can she get there quickly if she needs help?
- Is there a telephone or radio she can use in an emergency?
Work
- How much does she work at home and outside her home?
- Does she have time to rest?
- Does her work expose her to dangers — like chemicals? Can she be protected from work dangers?
It is important for the woman to get regular breaks from her work. She should be able to eat, drink, and urinate often. Her work should not put too much strain on her body.
Family
Partners and other family members can be supportive and can share in the responsibility of the pregnancy. They can help with housework, care for other children, help the woman get enough good food and rest, and can enjoy the growing pregnancy with the woman.
Some women need extra support
Women who do not have much family support, have no partner, or who have a partner who is not supportive may need extra care.
Single mothers are often wonderful and caring parents, but their lives may be harder than those of married women. People may treat single mothers badly, making assumptions about their morals and ignoring their needs. Give single mothers the kindness they deserve, and offer extra care if they do not have family or friends to help.
Very young mothers may have been forced into marriage as young girls, often to much older partners. These girls need particular support.
Women with abusive partners who get drunk or abuse drugs, are often away from home, have sex with other people, or abuse the woman will need support from family, friends, and you. A woman may need to leave her partner, or may choose to stay until she has a safe place to go. See the book Where Women Have No Doctor for more information on abusive partners.
Families save lives
Partners and family are usually the key to a good emergency plan. Find out if the woman needs permission to get medical help in an emergency. For example, if the community expects the husband to give the woman permission to go to a medical center or hospital, he should do so during the pregnancy, so that if he is away during the birth there will be no delay in getting life-saving care.
Teach the husband or partner, mother-in-law, or other close family members the warning signs that mean a woman must be taken to get medical help.
Community organizing for emergency care
Any woman can have serious problems that require medical help. If a woman has heavy bleeding, an infection, pre-eclampsia, or some other serious problem during labor or birth, she may need emergency care. A family with no car who lives far from medical help may have no way to get there. A family with little money may be unable to pay what the local hospital demands.
If everyone waits until a problem arises to think about how to solve it, the help may come too late. But with planning before the birth — while the woman is still pregnant — the woman, her family, her midwife, and her community can make a plan that can save the life of the woman or her baby. Make a transport plan before the birth with each woman. Involve her family and community in making the plan.
3 women last year. Do you know why?
A community transport plan should address all the reasons for delays in getting medical help. To understand these reasons, talk to other midwives who have lost mothers or babies during labor or birth. Talk to families who lost a baby or a mother too. Ask about when the midwife or family first knew there was a problem, and how long it took them to get help. Find out why the midwife and family did not go for help sooner. If possible, these families could meet and all talk to each other. Invite community leaders to listen to what these families and midwives have to say.
A midwife or a family might delay getting emergency care for many reasons:
- The person who must give permission for the woman to get care is not available.
- The midwife may feel afraid that people at the medical center will blame her for causing the problem.
- The family or the midwife may feel there is no hope — that going to a medical center will not help. Or the family may not trust the hospital.
- The family may not have money.
- There may be no car, truck, or other transportation.
After naming the reasons why families in the community do not get help, find solutions. You may be able to find a solution within the family. If the husband must give permission for the woman to go to the hospital, he can give permission in advance of the birth in case he is not home. Some problems are best solved by the whole community. In some villages, every family contributes a small amount of money every year. Anyone in the community who needs medical help can use the pool of money to pay for transportation to a medical center in an emergency.
Teach family members the warning signs. If everyone understands the problems that women in labor face, they can work together to help women get medical care. By talking to families and communities about the need for emergency medical care, you can help them make a plan that works. See Hesperian's Health Actions for Women for ways to begin these conversations.