Hesperian Health Guides
Malnutrition
Contents
Signs
- slow growth and small size
- thinness
- “wasting” of muscles: the body takes tissue from the muscles to supply energy
- slower thinking and lethargy, because the brain does not get the energy it needs
- more diseases and infections
- diarrhea happens frequently, making poor nutrition worse
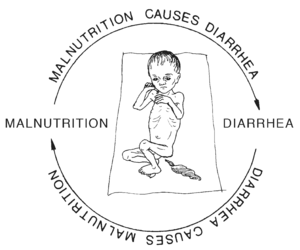
Malnutrition is common and often chronic. This means many people are hungry for long periods, so they never grow as tall as they might, they get sick more often than they should, and they get diarrhea, anemia, and other health problems more often.
Treatment
You can treat chronic malnutrition even when you do not have much, by giving more and better foods.
For babies from birth to about 6 months: give plenty of breast milk and nothing else. Any other food makes the problem worse. As the child grows, keep giving breast milk, and add other food too.
For everyone else with signs of malnutrition: give a high-energy porridge. Start by making a porridge with your main starchy food and add to it:
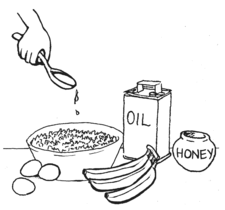
- Protein: Groundnut flour, peanut butter or another nut or bean flour or paste. Or cooked beans, eggs, or fish. Or milk, yogurt, or cheese. Choose any protein that is affordable and available to you.
- Energy: Add a spoon of oil and a spoon of sugar, honey, or another sweetener. Or add fruit.
- Vitamins and minerals: From cooked vegetables or fruit.
There may be times when there is not enough food to give a child a healthy meal with protein and vegetables every day. Still, try to avoid giving only starchy food with nothing else. With only starch, the child will feel full but will grow weak and sick. Add a spoon of oil. A spoon of oil does not make up for a lack of protein and vegetables. But for a short time it can give energy that a child cannot get from starch alone.
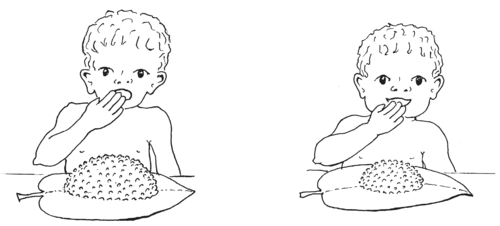 |
||
| To meet her energy needs, a child would need to eat this much boiled rice. | But when oil is mixed in, she needs to eat only this much. | |
Check all children for malnutrition
Chronic malnutrition in children often goes unnoticed. To check for malnutrition, weigh children regularly and keep track of their growth on a chart like the Road to Health Chart. If you do not have a scale, another way to check for malnutrition is to measure the child’s upper arm. Often there are programs or clinics for measuring the growth of children. These programs can be a good way to ensure a hungry child gets help early, before malnutrition becomes dangerous.
To measure the arm, cut a strip of paper, plastic, or cloth to about 25 cm.
Mark on your strip the places that show when a child is too thin, or has enough fat and muscle. At 0 cm write, “measure from here,” at 11.5 cm write “too thin,” and at 12.5 cm write “growing well.” Or use colors or symbols that make sense to you.
Use your strip to measure the upper arms of children between 1 and 5 years old, to make sure they are gaining enough weight. (Arm measurements are not useful when children have kwashiorkor, a kind of severe malnutrition that causes swelling in the arms and elsewhere.)
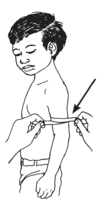
When a child’s arm measures less than 11.5 cm (below the “too thin” line), or she falls behind on the Road to Health Chart, or has signs of acute malnutrition listed on the next page, she is so malnourished that malnutrition has become an illness in itself. She needs urgent treatment and you can help save this child’s life by getting her high-energy food.
 | ||
| Note: this picture may print at different sizes, so use a ruler to make sure your strip has the correct measurements. | "too thin" line | YELLOW (in danger) If the child’s arm measurement is here she is at risk for becoming malnourished. Give her extra food, monitor her growth, and watch her closely so that she does not become malnourished. |
Severe, acute malnutrition
Severe, acute malnutrition happens in times of war, drought, or disaster when the food supply is interrupted. Or it can happen to someone who is poorly nourished most of the time, but something changes to decrease the food they eat or to increase the amount of energy they need. For example, when an already hungry child has a "growth spurt" and needs more energy . Or when a poorly nourished person gets HIV, malaria, leishmaniasis, measles, or some other sickness, and needs more food for energy to fight infection. Suddenly that "just enough" amount of food they were surviving on is no longer enough.
The information on malnutrition here is focused mainly on children because they suffer the most from it. They lose weight more quickly, and then lose their appetites, and must be given the most help to recover and survive. Without help, the damage caused by malnutrition can harm them throughout life. Adults get acute malnutrition too, and the treatment for adults is the same as for children.
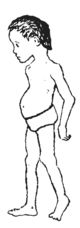
A severely malnourished child may look like this:
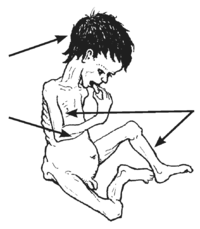 Hair that falls out easily
Dry, thin skin— the skin may seem loose
This kind of malnutrition is called marasmus.
Weak muscles, with wasting in the arms and legs
Very thin and small
|
Or a severely malnourished child might look like this:
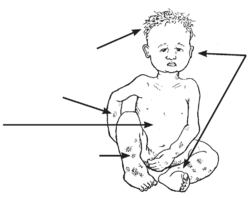 Dry, thinning hair loses its color and turns reddish, yellow or white
Peeling, cracked dry skin
Swollen belly
Sores or dark patches on the skin
This kind of malnutrition is called kwashiorkor.
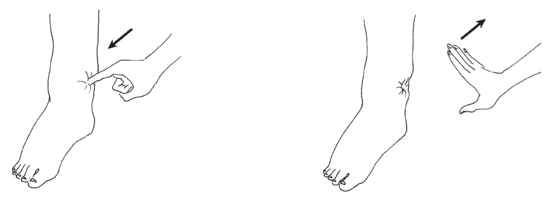
Swelling around the eyes or the feet or ankles
The child’s weight may be normal — he does not look thin
Exhausted or unwilling to move |
Sometimes children show a combination of signs from both kinds of malnutrition.
People with HIV, TB, worms, or other long-lasting illnesses may be malnourished even when they eat regularly. If a child or adult eats plenty of food but still looks malnourished, they may have a serious illness. An important part of staying healthy with any long-lasting illness is to eat more food. But also try to identify the cause of the problem.
 |
|
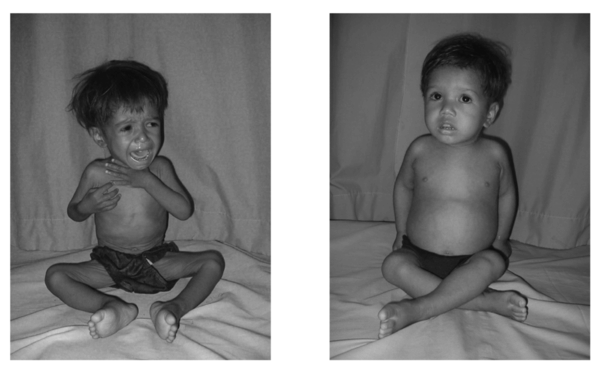
| Ashika was severely malnourished when she came to the clinic. | After a few weeks, good food had cured her. |
These two photos show the same 2 year old girl, Ashika. She came to the Nutritional Rehabilitation Home (NRH) in Kathmandu, Nepal with severe malnutrition. After 26 days of treatment with an enriched milk formula and a mixed diet of local foods, she gained enough weight to be healthy for her age, and went home with her mother. The NRH is not a hospital, just a big house with many beds, a vegetable garden, and a caring staff. They help around 20 children each month who suffer from severe malnutrition due to poverty, other illnesses, and lack of awareness about nutrition, as well as war and famine. Mothers also participate in their children's treatment. They learn about nutrition so they can help others when they return home. Feeding centers like these save the lives of most of the children brought to them.
Treatment for acute malnutrition
An acutely malnourished child needs medical help at once. If there is a feeding center in your area take the child there, or you may need to provide this care yourself. Give:
- food.
- drink (hydration).
- warmth, especially at night.
- medicines.
Food
Give highly concentrated food to quickly provide energy and nutrients. Plain starchy porridge is not enough.
You can make your own high-energy food at home. This homemade high-energy food is just as good as “therapeutic” foods such as Plumpy'nut and may be better in some ways. It is also a great food for any older baby or young child, because all young children need concentrated energy and nutrients to grow and be well.
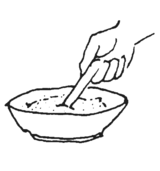
Combine 4 kinds of food using ingredients local to where you live: porridge, protein, fat or oil, and vegetable.
- Make 1 cup porridge from a starchy energy food.
Choose any one of these:
 Use whatever starchy food you usually make for your family, cooked into a thick paste (not a thin broth).
Use whatever starchy food you usually make for your family, cooked into a thick paste (not a thin broth).- millet
- maize
- rice
- wheat
- cassava
- yam or potato
- Add a high protein food.
Choose any one of these:
- 2 tablespoons milk powder
- 1 egg
- ½ cup roasted, pounded or ground seeds or nuts
- ½ cup cooked, mashed beans, lentils, or peas
- ½ cup cooked bean or pea flour
- ½ cup dried, pounded fish
- ¼ cup cooked, finely chopped meats or organ meats
- Add 2 tablespoons fat or oil.
Choose any one of these:
- any vegetable or nut oil, ghee, or lard
- Add ½ cup cooked vegetable.
Choose any one of these: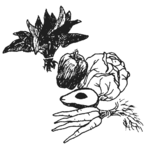
- tomato
- green leafy vegetables
- squash
- pumpkin
- green beans
- fresh peas
- okra
- or other vegetable
Give this high-energy porridge 4 or 5 times a day.
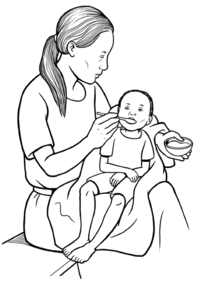
A malnourished child may not want to eat or may have energy to eat only very slowly. Offer a little food every hour or two. Be patient and persistent. Keep feeding this high-energy food to the child until she begins to gain weight and gets her energy and spirit back.
Wash your hands before cooking or serving food, use clean dishes, and use all the food you prepare in a day or so. Like any food, this high-energy food will eventually spoil, and will spoil faster if you live where it is hot.
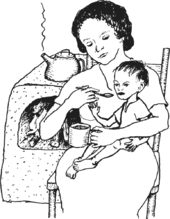
If the child is still nursing, breastfeed first and then give this high-energy food. Offer breast milk more often — because malnourished children may be too weak to nurse enough at each feed.
Also give fruit every day. Any fruit will give vitamins. But if you can, give different fruits on different days — so the child will get a variety of vitamins.
Fluids to drink (hydration)
Most malnourished children are also dehydrated from diarrhea. If a mother is breastfeeding, she should continue to give breast milk, as often as she can.
Along with breast milk, give rehydration drink. A child with severe malnutrition needs less salt and a bit more sugar than is in the usual recipe for rehydration drink. So:
 |
In 1 liter clean water | ||
| Mix ¼ teaspoon salt | |||
| Taste this mixture. It should be less salty than tears. | |||
| Then mix in 9 teaspoons sugar |  | ||
| Give spoonfuls of this mixture every few minutes. A malnourished person may not even have enough energy to drink. Support her head while you spoon the drink into her mouth. | |||
Warmth
With severe malnutrition, the body does not have the energy to warm itself enough. Check the person's temperature regularly. Warm her with blankets for several days, until she starts to recover. People get coldest at night, so she needs extra blankets then.
Medicines
Severe malnutrition is an illness and requires medicines. A severely malnourished child is likely to have infections. But her body is so weak, it may not be able to show the signs that usually tell us when someone is sick. For this reason, give medicines to fight infection, even if she has no fever or obvious infections. Give acutely malnourished children:
- amoxicillin or another antibiotic, 3 times a day for 7 days.
- measles vaccine (unless you are sure the child is already fully vaccinated against measles).
- vitamin A supplements.
- zinc supplements.
- mebendazole (if worm infections are common where you live).
Watch the child carefully
A malnourished child can quickly get much worse, and needs careful attention.
As you start giving fluids and food, check her heart and breathing rate (see Examining a Sick Person - in development). If these increase as you give rehydration drink, stop giving it and get medical help. Her heart may be having trouble adjusting to the fluid.
Is the child getting better? If she does not improve after a few days, she may have an infection or illness causing more problems. You probably need to go to a hospital. Also get help if at any time the child becomes unconscious (passes out), has a seizure, or has a fever, 38ºC (100.4ºF) or higher.
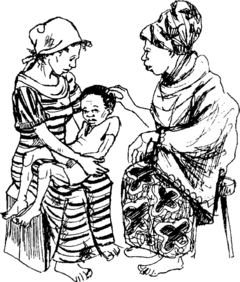
Help the child’s main caregiver understand exactly what this child needs to survive and get better. Clearly explain about rehydration, food, and any needed medicines as well as how to help the child eat more in the future. Remind the caregiver to be patient and persistent while feeding the child. Without attention to the child's food and care, she can quickly slip back into being malnourished. Ask the caregiver to explain the care instructions back to you, so you are sure they understand. And do what you can to help. Usually the care for a malnourished child is in the hands of a mother who is already busy watching other children and doing household work, and who lacks enough food herself. Helping the mother will help the child.
No matter how well she recovers, a child who has had severe malnutrition needs to be checked regularly to be sure her mind and body are growing and strong.
Ready-to-Use Therapeutic Foods
When people are starving, you may be able to get packaged, “Ready-to-Use Therapeutic Foods” (RUTF). These high-energy foods can be life-saving when you have nothing else, for instance, in refugee camps. But they have their problems. Dr. Massimo Serventi, a pediatrician in Tanzania, wrote to us about his concerns about Plumpy’nut, the best known RUTF:
(After being challenged by Médecins Sans Frontières, the company that makes Plumpy’nut did agree to allow local companies to make products using the Plumpy’nut recipe.)