Hesperian Health Guides
Malaria
HealthWiki > A Community Guide to Environmental Health > Chapter 8: Health Problems from Mosquitoes > Malaria
Malaria is an infection of the blood that causes high fever and chills. It is caused by a parasite (called plasmodium) that is passed to people by a certain kind of mosquito that bites mostly at night. Millions of people die from malaria every year, and many millions more live with the disease.
Malaria is especially dangerous to children under 5 years old, pregnant women, and people with HIV/AIDS. Pregnancy lowers a woman's ability to fight illness and infection. If she becomes ill with malaria, she may also get severe anemia (weak blood) which increases the chance of death during or after giving birth. Malaria in pregnancy can also cause her to lose the baby (miscarriage) or cause the baby to be born too soon, too small, or dead (stillbirth).
There are many kinds of malaria. People can live for many years with some kinds of malaria, and most kinds of malaria can be cured. But cerebral malaria (Plasmodium falciparum or P. falciparum) can cause death within 1 or 2 days of being infected. In areas where cerebral malaria exists, it is especially important to seek testing and treatment right away if you suspect you have malaria.
Usually malaria causes fevers every 2 or 3 days, but in the beginning it may cause fever every day. Anyone who suffers from unexplained fevers should have a blood test for malaria. This can be done at most health centers. If the blood test is positive for malaria, or if testing is not available, get treatment right away.
Signs
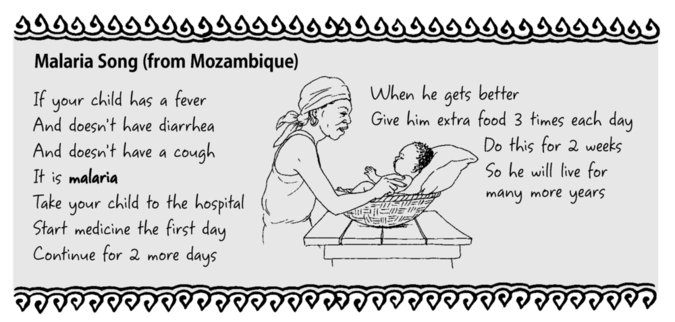
A malaria attack has 3 stages:
- The first signs are chills and often headache. The person shivers for 15 minutes to 1 hour.
- Chills are followed by high fever. The person is weak and at times not in his right mind (delirious). The fever may last hours or days.
- Finally the person begins to sweat and the fever goes down. After the fever drops, the person feels weak.
Treatment
If possible, get a blood test. Start treatment as soon as the first signs show. Because malaria is passed from person to person by mosquitoes, treating a sick person also protects others from getting infected. After you have been treated, mosquitoes that bite you will not pass malaria on to others.
Find out what medicines for malaria your local health authorities recommend. In many regions, the malaria parasite has developed drug resistance. This means that medicines that once worked to prevent or treat malaria are no longer effective. Medicines that cure malaria in one region may not cure the malaria found in a different place.
There are new medicines or combinations of medicines now being given to treat malaria in different regions. One of these, artemisinin (used for many years in China), is often taken with another antimalaria medicine or with an antibiotic. In some areas, chloroquine (the most common medicine for many years) still works. The only way to know what medicine will work in your area is to check with your local health authorities.
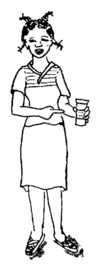 The woman who took all of her medicine got better. |
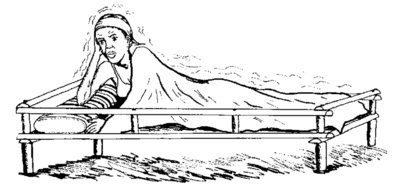 The woman who did not finish all her medicine is still sick in bed. |
Prevention
Malaria occurs most often during hot, rainy seasons because the mosquitoes that carry it breed in warm, stagnant water. But in some areas of the world, malaria is also found in the dry season, when mosquitoes find breeding sites in small standing pools of water. As with dengue and yellow fever, the best way to prevent malaria is to avoid mosquito bites and to use community mosquito control.
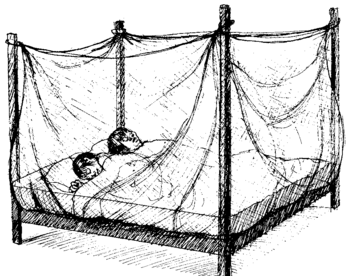
Sleeping under an insecticide-treated bednet is a good way to prevent and control malaria. These bednets are treated with an insecticide called “pyrethrins,” which is relatively safe, especially compared to getting malaria. The greatest dangers from insecticide-treated bednets are when they are dipped in the insecticide (leading to exposure through the skin), when children suck or chew on them (leading to exposure through swallowing), and when they are washed (because the insecticide can poison water sources and harm fish, insects, animals, and people downstream).
Bednets only protect if any holes or tears are quickly repaired. Also, the insecticide on the bednet wears off after 6 to 12 months, or sooner if it is often washed. In some places, you can now get "long-lasting" treated mosquito nets that work for over a year. If the bednet is still in good condition, new pesticide can be mixed and applied, but if the bednet has many rips or tears it may be safer to replace it. When reapplying pesticide, wear gloves and pay careful attention to the directions.
Treatment for all
Malaria is most common among poor people, and the number of deaths is growing each year. When people cannot afford blood tests and medicines and do not have access to health services, they are forced to live and die with this disease. And as long as one person has malaria, the infection can spread to others.
Malaria occurs most often in communities suffering from poverty and social injustice. For prevention campaigns to be successful, they must address the root causes of poverty and injustice as well as making treatment available for all.


