Hesperian Health Guides
Prevent Infections From Sex
HealthWiki > New Where There Is No Doctor > Sexually Transmitted Infections > Prevent Infections From Sex
- your partner has signs of an STI. They can easily pass the STI to you, or could have passed it already, even if you have no signs.
- you have more than one partner.
- you have a new partner who may have an STI from their previous partner.
- your partner has other partners who may have STIs.
- you and your partner do not use condoms.
- you have sex with someone who shares drug injection needles, or if you share needles to inject drugs.
Where testing is available, test often if getting a STI is possible. Testing for STIs every 6 to 12 months is a good idea for both women and men who have unprotected sex with more than one partner, with a partner who has sex with others, or because one person injects drugs.
Contents
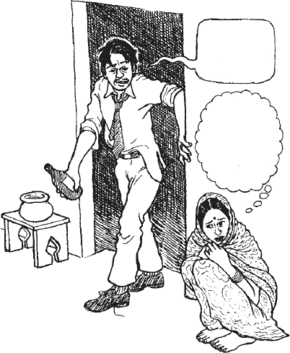
Women face more risks
Women face more obstacles to protecting themselves from STIs and getting adequate treatment, especially in communities where:
- child marriage is common.
- women are denied sexual health services and information.
- men are expected to have many partners.
- there is discrimination against people who are trans, making it harder for them to get health services.
- education is denied to girls and women.
- no one talks about sexual abuse or how to stop it.
- women are in situations where it is difficult or dangerous to refuse sex.
- sex work is criminalized.
- sex and sexuality are considered shameful, even though they are normal, and no one talks about sex openly.
 |
| Kissing is safe |
 |
| Touching is safe |
 |
| Oral sex is less safe than touching — but safer with a condom |
 |
| Vaginal sex is riskier than oral sex— but safer with a condom |
 |
| Anal sex is very risky— but safer with a condom |
Safer sex
What is safer sex and how can you make sex more safe for you? This may not be easy but often there is something you can do. Practicing safer sex can prevent you from getting or spreading a STI.
Here are some ways to have safer sex:
- Do not have sex. This is also called abstinence. If you do not have sex, you will not get a STI. Everyone can do this for a short while, but for most people this choice is not what they want for the rest of their lives.
- Have sex with only one partner. Choose a person you know for certain has sex only with you. Get tested together to make sure neither of you has a STI from a previous partner. Being faithful to each other and avoiding other ways of getting a STI will protect you both.
- Do not have sex with someone who has signs of a STI. Help them get tested and treated before you have sex with them. Unless the person gets tested, it is hard to know who has a STI and who does not. STIs can spread even if a person has no signs.
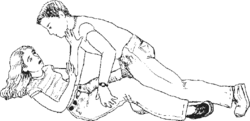
- Have sex with no penetration of the vagina or anus. There are many ways to give and get pleasure without penetration, including kissing, rubbing, or massaging different parts of the body, and touching each other’s genitals with the hands (mutual masturbation) or mouth (oral sex).
- Use condoms every time. Put on a latex condom before your partner’s genitals touch yours, every time, even with a long-term partner. Internal (female) condoms protect best against STIs because they cover more of the genital area. If you are trying to get pregnant, only have sexual intercourse without a condom during your fertile time. Use external (male) or internal (female) condoms (or dental dams or plastic wrap) during oral sex. Also use a condom with sex toys that more than one person has shared.
Talking about sex with a partner
Most people are taught not to talk about sex, even with the people they have sex with. Here are some suggestions:
- Focus on safety. If you want safer sex, your partner may think you do not trust them. But the issue is safety, not trust, because a person can have a STI without knowing it. Safer sex is a good idea for every couple, even if both partners have sex only with each other.
- Focus on preventing unwanted pregnancy. If you don’t want to have a child now, you and your partner can talk mostly about how condoms prevent pregnancy although they also prevent STIs.
- Practice talking with a friend. Ask a friend to pretend to be your partner and then practice what you want to say. Think of how your partner might respond, and practice for each possibility. It is likely you both will feel nervous talking about sex, so think of ways to make the conversation easier for each of you.
- Do not wait until you are about to have sex to talk about it! Choose a time when you are both relaxed and feeling good about each other. If you have stopped having sex because you have a new baby, or were being treated for a STI, try to talk before you have sex again. If you and your partner live far apart or one or both must travel often, talk about how to protect your sexual health before you get back together.
- Learn more about risks and how to have safer sex. People who do not know much about STIs, how they are spread, and their long-term health effects, cannot understand the risks involved in unsafe sex. Information can help you convince them of the need to practice safer sex.
Treatment as prevention
Most STIs can be cured with treatment, especially when treatment starts as soon as possible. Having one STI makes getting infected with HIV or other STIs more likely, but after treatment, people usually don’t spread STIs to others.
Treat right away. Health workers know their community and whether the person who has come to get help for a STI is likely to return for more care. That will help them decide which treatment or treatments to start with.
Treat partners. When you tell someone they have a STI, other people they had sex with will need to get tested and treated. If it is difficult for you to speak with former partners, health workers and STI programs can help contact the people so they get tested. If it is safe to speak with former partners, insist that they avoid all sexual contact until they are tested, treated, and cured.
Treating during pregnancy and treating quickly prevents passing the infection and the problems it can cause to the baby.
Preventive medicines for some STIs
Post Exposure Prophylaxis (PEP) is a way to use the medicines used to treat HIV, called antiretroviral treatment, to prevent a person from getting an HIV infection. When a person is exposed to HIV (for example, from rape or sex without a condom, or from syringe needles or contact with blood), taking HIV medicines as soon as possible within 3 days can prevent getting HIV.
When HIV medicines are taken daily by people without HIV to prevent getting HIV, this is called Pre-Exposure Prophylaxis (PrEP). See the chapter on HIV and AIDS (in development) for more information.
A full series of hepatitis B vaccine and hepatitis B immune globulin (HBIG), started as soon as possible after an exposure, can prevent hepatitis B infection.
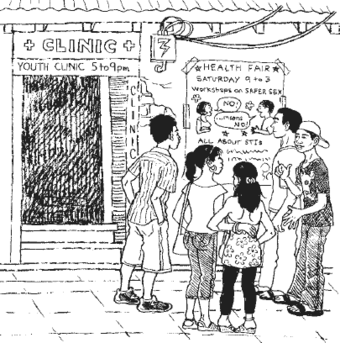
STI screening, testing, and treatment programs belong everywhere
When health centers provide STI testing and treatment as part of family planning services, pregnancy check-ups, and other health services, testing and treatment become more accessible to everyone. Everyone, especially young people, need accessible, affordable, and respectful services. Add services to school-based clinics or hold special events to offer testing and counseling at street fairs, bars, dance halls, or anywhere else to reach people who do not regularly get health care. Wherever people already go is a good place to bring STI information and services.
Discuss:
5 ways you can make people feel welcome
End shame and stigma about STIs
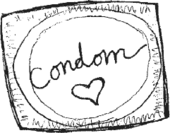
Share information about condoms and how to use them. Many clinics, government programs and non-governmental organizations provide free condoms to people who need them.
Work with your community. Talk and teach about sex. People are more likely to prevent STIs when they can talk about sex openly and have access to information, services, and condoms as well as testing and treatment for STIs. On the other hand, where sex is considered to be shameful, it is more difficult for people to learn about STIs or seek help. Hesperian’s Health Actions for Women has many activities and ideas to start conversations and solve problems related to sexual health.
If couples with same sex relationships (between 2 men, or between 2 women) are discriminated against or hidden, people will have a harder time talking with their partners about safer sex, testing, or seeing a health worker.
Stigma or discrimination against sex workers, people who inject drugs, have dark skin, or are members of a “lower” class or caste, make it that much harder for the community to prevent STIs.
Health centers can help lessen the stigma of having a STI by providing testing and treatment as a routine part of health care for all adults and young people. For people to be comfortable with STI testing, they need to know they will be treated with respect and privacy.
In the long run, STIs can best be prevented by fighting for fairer social and economic conditions. When families do not need to separate to find work, when people need not trade their bodies for food, shelter or money, and when young people have access to education and a future, there will be fewer cases of sexually transmitted infections.