Hesperian Health Guides
Improve access to care for pregnant women
HealthWiki > Health Actions for Women > Chapter 8: Healthy Pregnancies and Safe Births > Improve access to care for pregnant women
Contents
Plan for the birth
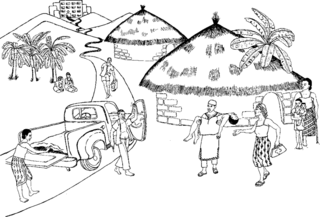
A pregnant woman should be able to make her own decisions about where and how she wants to give birth, but she also needs the support of her family and community, and support from the health workers who assist her with the birth. In many families, it is especially important to include men, mothers-in-law, and other family elders in making a birth plan. These are the people who will be nearby, will be able to help, and may also control the family’s money or vehicle.
These are some questions that can help a woman and her family make a birth plan:
- Where will the birth take place? Will she have to pay fees? How much? Who will pay?
- What supplies are needed, and who will provide them?
- How will she get there? Does the woman need transportation? How much will it cost, and who will pay?
- Who will take care of her other children, her crops, and her animals while she is in labor and recovering after the birth?
Prepare for emergencies
Any woman can have an emergency during pregnancy or birth. In case of emergency, a woman needs to be able to get medical care within 2 hours. Planning for emergencies means being able to act quickly, get help, and save the life of the woman and her child. During the last weeks of pregnancy, if the hospital is too far away to reach in 2 hours, a woman can stay with a friend or family member who lives closer to a hospital.
The 4 delays
Some problems during pregnancy or birth can become very dangerous very quickly. Four common delays in getting help make the danger worse. These delays must be shortened to prevent women from dying:
- A delay in seeing the danger. People may not know enough about birth and the signs of danger during birth. They do not see that something is wrong, so they do not act quickly enough to help. Learn about danger signs.
- A delay from taking too long to decide to get help. People may know something is wrong, but they do not decide to get help quickly enough. Many people are not ready for emergencies. They may not have transportation or money to pay doctor or hospital fees.
- A delay from taking too long to get to the hospital. The hospital may be very far away, or the trip may take too long for other reasons.
- A delay in getting care at the hospital. The hospital may not have the supplies or trained staff it needs to save women’s lives. There may be communication problems, especially if the nurses and doctors do not speak the woman’s language. Health workers who do not treat women with respect often leave them waiting too long for care.
Use an activity such as the "But why?" game to help people gain a deeper understanding of each of the 4 delays and to feel less overwhelmed by them. When you ask, "But why don’t people see the danger?" and they answer, "Because they don’t know the danger signs," you can begin to expose the root causes and get ideas about how to organize people to address these problems.
Barriers to prenatal and emergency care
Why do women not get health care when they need it? There are many reasons why women do not get good prenatal care, do not plan for emergencies, or wait too long to get medical care when their lives are in danger. The stories Never again! How a needless death became a call for change and Vanna's unsafe pregnancies include examples of common reasons. In those stories, both women were afraid to go to the nearest clinic, health center, or hospital. They did not feel welcome in those places, and they did not trust the health workers to treat them kindly and with respect.
If women in your community are afraid or unwilling to go to a health center or hospital, try to find out why. When you know the reasons, you may be able to work with community leaders and people at the health center to make changes and gain the community’s trust.
Role plays can be a good way to help a group look more deeply at the different barriers that keep pregnant women from getting the care they need. Here are some examples of situations that can be used to create theater and role plays about why pregnant women do not go for care. (It is best to prepare these scenarios ahead of time.) For more information about role plays, see Role plays to discuss gender-based violence and Teaching with drama.
A 15-year-old girl finds out she is pregnant, and she is afraid of what will happen when her parents find out. The nurse at the health center is very religious, and talks with parents when their daughters come to the health center looking for family planning.
A woman is pregnant. She already has 5 children. Her husband is away in another country trying to earn money because he could not find a job at home. He has not been able to send money home yet, and she is having a very hard time getting enough food to feed her children. She did not have problems with the births of her other children, so she hopes things will go OK with the birth of this baby.
You can also prepare a skit or play using the information in the story, Vanna's unsafe pregnancies.
Activity
Role play why pregnant women do not get care
- Divide the participants into several smaller groups of about 5 people each and ask each group to spend 15 to 20 minutes preparing a 5 minute play. Each group presents their role play for the other participants. Encourage everyone to play a part.
-
To help the groups prepare their skits you can ask them to think about questions like:
- How would the woman be treated by the staff at a health center? Would she be treated differently than others? How are unmarried women treated?
- How long might she have to wait to see a health worker? What are the hours that the health center is open?
- How much do services cost? Does everyone pay the same for the same services? Do staff expect bribes or charge extra fees?
- How far away is the health center?
- What does the health center look like? How it is supplied?
- Who do pregnant women prefer for care before, during, and after birth? Why do they prefer that person or those people?
- Have each group perform their skit.
- Once all the actors have stepped out of character, discuss what barriers prevent women from seeking and receiving the care they need.
- Conclude this activity with Head, Heart, Hands. This helps people reflect on what they have learned by examining thoughts (head), looking at feelings (heart), and considering what to do about it (hands). In this case, you want participants to identify changes to make at the hospital or health center that would make it easier for all pregnant women to get the care they need.
Health problems that require extra care
Some women should always try to give birth in a medical center or hospital, even if they have regular check-ups with no danger signs during pregnancy. This includes women who:
- are under age 17 or over age 35.
- have had more than 5 births.
- are sick or who may have anemia (blood weak from lack of iron) because they have not had enough healthy food to eat.
- have diabetes (too much sugar in the blood).
- had problems with a previous pregnancy and birth, such as severe bleeding, high blood pressure, or very long or obstructed labor.
- had a previous birth by Cesarean section.
A woman with HIV may be able to have a birth that is safer for her baby at a hospital.
Birth by operation (Cesarean section, C-section)
Most women are able to give birth naturally, through the vagina. But this can be dangerous for a woman or her baby under certain conditions, such as when the baby is in a difficult birth position and cannot pass through the vagina, or when the woman is bleeding, has eclampsia or a severe infection, or if the opening to the woman’s vagina was made very small after genital cutting. When complications like these make it dangerous for a woman or her baby to go through normal labor and birth, a cut is made in the woman’s belly so her baby can be born.
A C-section is sometimes necessary to save the life of a woman and her baby. But too often they are done because they are easier for the doctor or the hospital — not the woman — and the doctor can control everything that happens.
Obstetric fistula: a preventable injury
Some women who survive a long, difficult labor suffer afterward from a serious injury called called obstetric fistula. The fistula is a hole in the woman’s vagina caused by a baby’s head pushing hard in the same spot for a long time. After the birth, urine or stool leak through the hole and out of the woman’s body through her vagina. There is nothing she can do to control the leak. Women with fistula are usually confined to their homes. They are often abandoned by their families and stigmatized in their communities.
Fortunately, fistulas can be repaired with an operation. They can also be prevented. Fistulas are rare in places where pregnant women get regular check-ups by trained health workers and give birth in a well-equipped clinic or hospital if their labor is too long. Fistulas occur most frequently in places where girls marry when they are very young and get pregnant before they are fully grown, and also in places where genital cutting is common.
Preventing fistula and healing lives in Pakistan
Women in rural communities in Pakistan suffered the shame of fistulas for many years. Now, doctors and midwives are helping people in those communities understand the true cause of the problem and stop believing the myth that fistula is a curse. A male doctor, Shershah Syed, founded Koohi Goth Hospital for Women in Karachi, and led a public education campaign to raise funds to provide care for over a thousand women who suffered from fistula. An actress, Shema Kirmani, uses community drama to raise awareness about fistula and maternal mortality, and to explain how to get treatment to repair fistula.
These efforts to prevent fistula and help women get early treatment have resulted in fewer women suffering from this problem. Community education and public dialogue have also reduced stigma. Midwives and village leaders involved in raising awareness about fistula became connected to national and international struggles for women’s rights and human rights. These connections have given them stronger skills to advocate for safe motherhood and women’s rights in Pakistan. Similar work to promote women’s rights and human dignity is happening in 40 other countries in Africa, South Asia, and the Middle East.


