Hesperian Health Guides
Medicines to Prevent Seizures
HealthWiki > Disabled Village Children > Chapter 29: Seizures: Epilepsy > Medicines to Prevent Seizures
As long as a child has epilepsy—which may be for a short time or for their entire life—they must take anti-seizure medicines to control their seizures and prevent further injury.
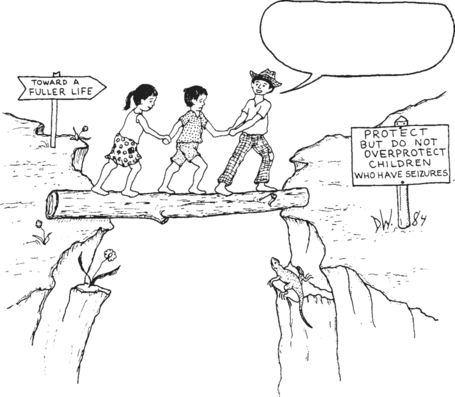
It is important that epileptic children go to school and take part in day-to-day work, play, and adventures in family and village life. This is true even if seizures are not completely under control. The schoolteachers and other children should learn about epilepsy and how to protect a child when she has a seizure. If they learn more about epilepsy it will help them to be supportive rather than afraid or cruel. (See "CHILD-to-child activities".)
Choosing medicines
|
The best medicine (or medicine combination) for a child with epilepsy is one that is:
|
CAUTION! Great care is needed to select the medicines that help the individual child most, and which do her the least harm. Try to avoid giving so much medicine that she always seems sleepy, dizzy, slow-moving, or loses interest in things. A few seizures may be better than too much medicine—which can poison the child which can weaken learning, prevent the child from participating in social interactions, and can even worsen seizures in some children. |
When children with epilepsy take their medicine regularly for an extended time and successfully prevent having seizures, sometimes the medicine can be stopped and the seizures will not return. To make it more likely, the child should take anti-seizure medicine for at least a year after their last seizure. They can then take a gradually lowered dose and finally stop the medicine, usually over weeks or months. Always lower the dose and stop the epilepsy medication gradually. However, if seizures return, medicines should be restarted, at least for another year before trying to stop again.
WARNING! Abruptly stopping medicines can cause seizures to return quickly, perhaps more strongly than before.
The best medicine to try first for almost all types of seizures among children is usually carbamazepine. It is very effective and is relatively safe, cheap, and easy to take. Usually, it is given to children in 2 doses every day.
The next best medicine for generalized seizures is usually valproate. It is also fairly safe, cheap, and usually needs to be taken in 2 doses every day. Phenobarbital and phenytoin are also cheap and easily available medicines. However, phenobarbital may cause learning delay in young children. Phenytoin can also cause side effects, such as swelling or too much growth of the gums or a flattening of facial features among young children. It can also worsen generalized seizures for some children.
Sometimes, only a combination of medicines can stop a child from having seizures. A second drug may be added after the peak dose of the first drug is reached. Any new medicine should be added in consultation with a doctor or a health worker. Some doctors prescribe more expensive, harder to get, less safe and often less effective medicines before trying the medicines mentioned above. Partly this is due to drug companies advertising their more expensive products. Also, in some countries, phenobarbital is difficult to get in pill form. The result is that many children’s seizures are poorly controlled, using costly drugs that cause severe side effects. Rehabilitation workers need to realize this and do what they can to help provide the safest, cheapest medicines that will effectively control a child’s seizures.
It is usually best to start with only one anti-seizure medicine, usually carbamazepine or valproate. If these medicines are not available, try phenobarbital or phenytoin. Start with a low to medium dose, and if after a week seizures are not controlled and there are no serious side effects, increase to a higher dose. After a few days, if the seizures are still not controlled, consult a health worker about whether and how to add a second medication. Always start with a low to medium dose and gradually increase as needed.
Note: Taking the medicine at the same time(s) every day can help maintain the same amount of drug in the blood. It can also make it part of a child’s routine and help the parent or caregiver to remember to give the medicine.

WARNING! All anti-seizure medicines are harmful if a child takes too much. Be careful to give the right dose and to keep medicines out of reach of children.
| INFORMATION ON DOSAGE AND PRECAUTIONS FOR ANTI-SEIZURE MEDICINES | |||
|---|---|---|---|
| Carbamazepine (Tegretol) | |||
| Useful for many types of seizures as a first choice, or in combination. Especially useful for psychomotor seizures. | |||
| Usually comes in: tablets of 100 mg or 200 mg | |||
| Dosage: Usually given 2 times a day. Give with food. Start with these doses: | |||
| children under 6 years | 5 mg/kg/day, or 50 mg by mouth 2 times a day. | ||
| If necessary, increase dose weekly by 5 mg/kg/day but never give more than 30 mg/kg/day. | |||
| children 6 to 12 years | 100 mg by mouth, 2 times a day | ||
| If necessary, increase dose weekly by up to 100 mg per day until seizures stop. | |||
| children over 12 years | 200 mg by mouth, 2 times a day | ||
| If necessary, increase dose weekly by up to 200 mg per day until seizures stop. | |||
| The dose of carbamazepine should be adjusted to the individual child. Try to give the lowest amount of medicine that stops the seizures. A dose that is too high can cause dizziness, unsteady walking, or vomiting. | |||
| Side effects & complications: | |||
| If a skin rash develops 2 to 8 weeks after starting carbamazepine, talk to a health worker about changing to a different medicine. | |||
| Valproate (Depakene) | |||
| Used alone or in combination with other anti-seizure drugs for focal seizures with absences, especially group seizures. Do not use with carbamazepine. | |||
| Usually comes in: tablets of 100 mg or 200 mg | |||
| Dosage: Usually given 2 or 3 times a day. Start with these doses: | |||
| children under 6 years | 10 mg/kg/day, or 100 mg by mouth 2 times a day. | ||
| Use with extreme caution and as the only medicine. If necessary, increase dose weekly by 5 mg/kg/day but never give more than 60mg/kg/day. | |||
| children 6 to 12 years | 200 mg by mouth 2 times a day | ||
| If necessary, increase dose weekly by up to 100 mg per day until seizures stop. | |||
| children over 12 years | 300 mg by mouth 2 times a day | ||
| If necessary, increase dose weekly by up to 200 mg per day until seizures stop. | |||
| The child may gain weight. Some children develop liver problems, signs of which include sudden loss of appetite, jaundice in the eyes, or change in the color of urine. People who could get pregnant should not use this medicine. | |||
| Phenytoin (diphenylhydantoin, Dilantin) | |||
| For many types of seizures, but not for absence seizures. Phenytoin may make these kinds of seizures worse. | |||
| Usually comes in: capsules or tablets of 25 mg, 50 mg, and 100 mg syrup with 30 mg in each 5 ml (1 teaspoon) | |||
| Dosage: Usually given 2 times a day. Start with these doses: | |||
| under 6 years | 3 to 5 mg/kg/day, or 25 mg by mouth 2 times a day | ||
| 6 to 12 years old | 75 mg by mouth, 2 times a day | ||
| If necessary, increase after 2 weeks by 25 mg a day until seizures stop. | |||
| children over 12 years | 100 mg by mouth, 2 times a day. | ||
| If necessary, increase after 2 weeks by 25 mg a day until seizures stop. | |||
| After 2 weeks, if the seizures are not completely prevented, the dose can be increased little by little, but not to more than twice the starting amount. The difference between not enough and too much can be very small. If child has no seizures during several weeks, try lowering the dose little by little until you find the lowest dose that prevent the seizures. | |||
| Side effects & complications: | |||
| Watch for dizziness, eye-jerking, slurred speech, seeing double, and drowsiness. Lower the dose if any of these early signs of poisoning occur. They could cause permanent brain injury. | |||
|
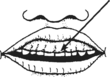
very swollen, sore gums almost covering teeth—caused by not keeping teeth clean while taking phenytoin | ||
 | |||
|
WARNING! Sudden stopping of phenytoin may cause the child to have a long-lasting seizure. Be sure to lower the dosage gradually when stopping or changing any epilepsy medicine. | |||
| Phenobarbital (phenobarbitone, phenobarb, Luminal)) | |||
| For all types of seizures. Usually comes in: | |||
| 15 mg, 30 mg, 50 mg, 60 mg and 100 mg and syrup with 15 mg in each 5 ml (1 teaspoon) | |||
| Dosage: Usually given by mouth 2 times a day, but a double dose can be given 1 time a day at bedtime. | |||
| children under 7 years | 3 to 5 mg/kg/day, or 10 to 25 mg by mouth 2 times a day. | ||
| children 7 to 12 years | 25 to 50 mg by mouth, 2 times a day | ||
| children over 12 | 50 to 150 mg by mouth, 2 times a day | ||
| Some children do better with 1 dose a day instead of 2 doses. Give twice the amount listed here at bedtime. But if the seizures return or the child has problems going to sleep or waking up, go back to 2 doses a day of the regular amount. | |||
| SIDE EFFECTS AND COMPLICATIONS | |||
| |||
|
CAUTION! Giving too much can poison the child. | |||
OTHER DRUGS SOMETIMES USED FOR EPILEPSY
- Ethosuximide (Zarontin) First choice for absence epilepsy, especially if seizures occur in groups in the morning and evening. The initial dose for children between 3 to 6 years of age is one capsule (250 mg) per day; for children 6 years and older, two capsules (500 mg) per day. Give with food to avoid stomach ache. Rarely, causes liver damage.
- Corticosteroids (or corticotropin) These are sometimes tried for baby spasms and myoclonic seizures that are not controlled by other medicines. Long-term use of these medicines causes serious and possibly dangerous side effects. They should be used only with highly skilled medical advice when all other possible medicines have failed.
- Diazepam (Valium) Sometimes used for newborn seizures or baby spasms, but other medicines should be tried first. It can cause an increase in the number and severity of generalized tonic-clonic (grand mal) seizures. May cause sleepiness or dizziness. Habit forming. Start with about 1 to 2.5 mg, 3 or 4 times daily. Do not give to children under 6 months.
TREATMENT FOR A LONG-LASTING SEIZURE
When a seizure has lasted more than 5 minutes:
- if someone knows how, inject IV diazepam (Valium) or phenobarbital into the vein or, using a syringe with no needle, in the rectum.
| Doses for injectable diazepam: | ||
| Adults | 5 to 10 mg | |
| Children 6 to 12 years | 3 to 5 mg | |
| Children under 6 | 1 mg for every 5 kg of body weight | |
| Doses for injectable phenobarbital: | |||||
| Adults | 200 mg | ||||
| Children 6 to 12 years | 150 mg | ||||
| Children 2 to 6 years | 100 mg | ||||
| Children under 2 years | 50 mg | ||||
Note: These medicines do not work as fast or well when they are injected into a muscle. If you only have injectable or liquid medicine, put it up the rectum with a plastic syringe without a needle. Or grind up a pill of diazepam or phenobarbital, mix with water, and put it up the rectum.
If the seizure does not stop in 15 minutes after giving the medicine, repeat the dose, but do not repeat more than once.


