Hesperian Health Guides
Choosing a family planning method
- Does she want to be very sure she will not get pregnant?
- Is she concerned about side effects (uncomfortable or unintended effects)?
- How does she feel about a method that must be remembered each day? Or methods that involve touching her genitals?
- Is the woman’s partner willing to participate in using family planning?
- Which methods of family planning can this woman afford?
- Does the woman want a method that she can stop using if she wants to become pregnant? Or one that is permanent?
- Is prevention of sexually transmitted infections (STIs) also important?
The methods described in this chapter work well to prevent pregnancy. Each of these methods also has disadvantages. The woman and her partner may need instruction on how to use the method. The method may cost something, it may require a medical visit, or it may have certain health risks. Make sure you understand how comfortable, safe, costly, or complicated each method is before you recommend it. Make sure the woman understands too.
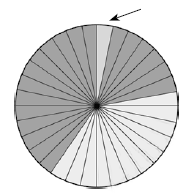
The chart below shows how well each method works to prevent pregnancy and to protect against STIs. The chart also shows possible side effects for each method and other important information about how the method must be used. Each method has stars to show how well it prevents pregnancy for the average user. When people use a method correctly every time they have sex, the method will work better.
| FAMILY PLANNING METHOD |
Protection from Pregnancy |
Protection from STIs |
Possible side effects |
Other important information |
|
|---|---|---|---|---|---|
| External condom (male condom) |
★★ GOOD |
 GOOD |
Most effective when used with spermicide and waterbased lubricant. Prevents STIs when used alone or with other methods. | ||
| Internal (female) condom |
★★ GOOD |
 GOOD |
Most effective when used with spermicide and waterbased lubricant. Prevents STIs when used alone or with other methods. | ||
| Diaphragm or cervical cap (with spermicide) |
★★ GOOD |
SOME |
Most effective when used with spermicide. Effective only when using the correct size | ||
| Hormonal Methods Birth control pill, patch, injections, vaginal ring 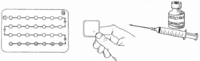 Implants  |
★★★ |
NONE |
Nausea, headaches, changes in monthly bleeding |
These methods should not be used by women with certain health problems. | |
| IUD copper or hormonal 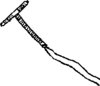 |
★★★★ BEST |
NONE |
heavy and painful monthly bleeding |
This method should not be used by women with certain health problems. | |
| Sex that doesn’t cause pregnancy (penis not inside vagina at all)  |
★★★★ BEST |
SOME |
Sexual touch rarely passes STIs. Oral sex is less likely to pass STIs. Anal sex easily passes STIs. | ||
| Breastfeeding (during the first 6 months only)  |
★★★ VERY GOOD |
NONE |
Only effective in the first 6 months after birth, if giving baby only breast milk, and if periods have not returned. | ||
| Fertility awareness  |
★★ GOOD |
NONE |
Only effective for people who can choose not to have penis-in-vagina sex. | ||
Sterilization  |
★★★★ BEST |
NONE |
A person will never be able to have babies after this operation. | ||
| Pulling out (withdrawal)  |
★ SOME |
SOME |
More effective when used with another method like spermicide or diaphragm. | ||
Contents
- 1 External condom (male condom, rubber, prophylactic)
- 2 Internal condom (female condom)
- 3 Diaphragm
- 4 Spermicide (foam, jelly, cream, tablets, or in sponges)
- 5 Hormonal methods (pills, injections, implants, patches, vaginal rings, hormonal IUDs)
- 6 Intrauterine devices (IUDs)
- 7 Abstinence and sex that does not cause pregnancy
- 8 Breastfeeding to prevent pregnancy (Lactational Amenorrhea Method, LAM)
- 9 Fertility awareness (natural family planning)
- 10 Sterilization
- 11 Emergency contraception: Pills
- 12 Emergency contraception: IUDs
- 13 Pulling out (withdrawal)
- 14 Contraceptive sponge
- 15 New methods of family planning
- 16 Methods that do not prevent pregnancy
External condom (male condom, rubber, prophylactic)
An external condom is a narrow bag of thin rubber that the man wears on his penis while having sex. The bag traps the man’s sperm (seed) so that it cannot get into the woman’s vagina or womb. Condoms work well to prevent pregnancy. Condoms also help prevent sexually transmitted infections (STIs), including HIV.
The most effective condoms are made from latex or polyurethane, not sheepskin.
A new condom must be used each time a couple has sex.
Lubricant can make sex feel better for both the woman and the man. It can also keep the condom from breaking. Use a water-based lubricant like saliva (spit), K-Y Jelly, or spermicide. Do not use oils, petroleum jelly (Vaseline), skin lotions, or butter. They can make the condom break. A drop of lubricant inside the tip of the condom makes it more comfortable on the penis. A little lubricant can also be rubbed on the outside of the condom after the man puts it on.
Internal condom (female condom)
An internal condom fits into the vagina and covers the outer lips of the genitals. The internal condom is the most effective of the methods controlled by women in protecting against STIs, including HIV.
Each condom should be used only once, because it may break if it is reused. But if a woman does not have any other condoms, she can clean it and reuse it up to 5 times. An internal condom should not be used at the same time as an external (male) condom.
Internal condoms can be expensive and take time to learn to use. Several types of internal condoms are now available, including versions made of plastic (like the FC2 and the Woman’s Condom), and latex (like the VA and the Cupid Condom).
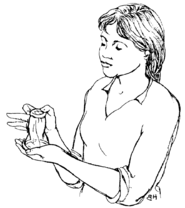
How to use an external (male) condom
A new condom should come rolled up inside a small packet that has not been opened. Be careful not to tear the condom as you open the packet. If the condom is stiff, hard or feels sticky, throw it away. It will not work.
|
1. A condom should be put on the man’s penis when it is hard, and before it touches the woman’s genitals. An uncircumcised man should pull his foreskin back. The man should squeeze the tip of the condom and put it on the end of the penis. |
 |
| 2. Unroll the condom until it covers all of the penis. Keep squeezing the tip of the condom while unrolling. Without this extra space at the tip for the sperm, the condom may break. | 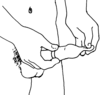 |
| 3. Right after the man ejaculates (comes) and before his penis gets soft, he should hold on to the rim of the condom while he pulls his penis out of the vagina. Then he should carefully take the condom off. | 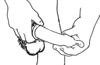 |
| 4. Put it in the garbage or a latrine; do not flush it down a toilet. | 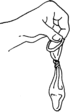 |
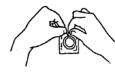
How to use an internal (female) condom
|
1. Carefully open the packet without tearing the condom. |
 |
|
2. Find the smaller inner ring, which is at the closed end of the condom. |
 inner
ring outer ring |
| 3. Squeeze the inner ring together. | 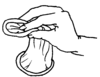 |
| 4. Put the inner ring in the vagina. | 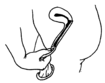 |
| 5. Use your finger to push the inner ring up into your vagina and over the cervix. The outer ring stays outside the vagina. | 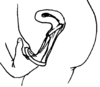 |
|
6. Be sure to guide the penis through the outer ring when you have sex. |
 |
| 7. Remove the internal condom immediately after sex, before you stand up. Squeeze and twist the outer ring to keep the man’s sperm inside the condom. Pull the condom out gently, then bury it or throw it in a latrine. Do not flush it down the toilet. |
Diaphragm
The diaphragm is a shallow cup of soft rubber or silicone that is put into the vagina before sex. It prevents pregnancy by covering the cervix so sperm can’t get into the womb. Diaphragms work best with spermicide. It is moderately effective in preventing pregnancy and may also give some protection against STIs, like HIV.
Many diaphragms come in different sizes, and a health worker must help a woman find the right size. Midwives can learn to do this. A “one size fits most” diaphragm (Caya) is becoming more available and does not require a fitting by a provider.
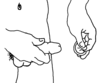
How to Use a Diaphragm
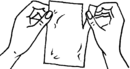
| 1. Squeeze some spermicide into the center of the diaphragm. Then spread a little around the edge of the diaphragm. If you do not have spermicide, you can still use the diaphragm, but it may not work as well. | 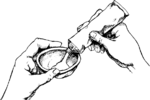 |
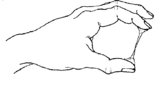
2. Squeeze the diaphragm in half. | |
 | |||
| 3. Push the diaphragm into the vagina, toward your back, right over the cervix. |  |
If the diaphragm is in correctly, the woman can feel her cervix through it. It feels like the end of your nose. |
 |
|
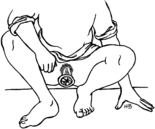
4. Leave the diaphragm in place for at least 6 hours after sex. If the woman has sex again before 6 hours have passed, she should put more spermicide in her vagina first. After using the diaphragm, the woman should wash it in mild soap and water. Then she should dry it, dust it in cornstarch if she has any, and store it in a clean, closed container | |||
Spermicide (foam, jelly, cream, tablets, or in sponges)
A spermicide is a chemical that kills sperm after it comes out of the penis. Spermicides are fairly good at preventing pregnancy when used alone and are more effective when used with a condom or diaphragm.
WARNING! Do not use spermicide if you or your partner have HIV. Most spermicide is made with the chemical nonoxynol-9. Nonoxynol-9 irritates the vagina, causing tiny cuts that allow HIV to pass more easily into the blood. So using spermicide, especially using it very often, may make HIV more likely to pass during sex.
How to Use Spermicide
 cream or jelly |
 applicator
foam |
 tablets |
The woman puts the spermicide foam or jelly in her vagina with an applicator. Tablets (suppositories) are put deep in the vagina with the fingers.
Tablets must be put in the vagina at least 10 minutes before sex to have time to dissolve. Foam and jelly can be put in the vagina just before sex. If more than 1 hour passes between inserting spermicide and having sex, more spermicide is needed — a new tablet or applicator of foam or jelly. Also add more before each time you have penis-in-vagina sex again.
Hormonal methods (pills, injections, implants, patches, vaginal rings, hormonal IUDs)
Hormones are a type of chemicals our bodies make. They regulate many body processes, including monthly bleeding and the ability to become pregnant. Hormonal family planning methods prevent pregnancy by thickening the mucus in the cervix so sperm cannot pass through. Some methods also prevent the ovaries from releasing eggs. Hormonal methods include:
 |
 |
 |
| pills | injections | implants |
 |
 |
 |
| patches | vaginal rings | hormonal IUD |
Hormonal methods prevent pregnancy very well, but do not protect against HIV or other STIs.
Most birth control pills, the patch, the vaginal ring, and some injections contain 2 hormones: estrogen and progestin. Implants, hormonal IUDs, some pills, and some injections contain only progestin.
Side effects
Hormonal methods sometimes have side effects. These effects are not dangerous, but they are often uncomfortable. Hormonal methods can make a woman have:
| nausea | headaches | weight gain | swelling of the breasts |
changes in monthly bleeding |
 |
 |
 |
 |
 |
These effects usually get better after a few months. If they do not get better, the woman can try a different family planning method.
Birth control pills (oral contraceptives or "the pill")
When a woman takes a birth control pill at the same time every day, this is an effective way to prevent pregnancy.
There are many brands of birth control pills with different amounts of estrogen and/or progestin in them. Most pills have 1 milligram (mg) or less of progestin and 35 micrograms (mcg) or less of estrogen.
How to Take Birth Control Pills
If a woman is sure she is not pregnant, she can start taking the pill at any time. Pills can also be started the same day as or at any time in the first 7 days after an abortion or miscarriage.
Most pills come in packets of 21 or 28 tablets. Always check a new packet of pills to make sure the pills of the same color all look the same, none are crushed or broken, and the packaging is intact. If not, return them for another packet.
A woman using a 28-day packet should take one pill every day. Women will usually have light monthly bleeding during the last 7 days of a pill packet. As soon as she finishes one packet, she should begin taking a new one.
The last 7 pills in a 28-day packet contain sugar instead of hormones, but help someone remember to take a pill each day. If a woman prefers not to bleed every month, it is safe to take only the hormone pills continuously for up to 3 months. When the woman reaches week 4 of her packet (the sugar pills), she can immediately begin a new packet of pills instead of taking the sugar pills. Then continue taking the hormone pills in the usual order.
Pills will not prevent pregnancy until a woman has been taking them for about a week. So during the first 7 days after starting birth control pills, she should use condoms or another barrier method or avoid penis-in-vagina sex.
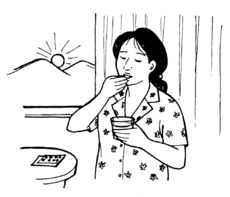
It is best to take the pill at about the same time every day. Many women take the pill with food, especially if they feel some nausea during the first few months they take it.
What if a woman forgets to take her pill?
If a woman misses or is late taking 1 pill, she should take the late or missed pill as soon as she remembers, and then take her next pill at the regular time — even if this means taking 2 pills in one day.
If she forgets to take 2 or more pills in a row, she should take the most recent pill as soon as she remembers and discard any other missed pills. She should take the remaining pills in the pack at the regular time, even if this means taking 2 pills in one day. If she missed pills in the last week of hormonal pills (days 15 to 21 in a pack), she should finish the hormonal pills in the current pack, skip the sugar pills (or the 7 day wait for a 21-day pack), and start a new pack
To prevent pregnancy, she should use condoms or another barrier method every time she has penis-in-vagina sex until she has taken hormonal pills for 7 days in a row.
forgot!
If a woman often forgets to take her pills, she may be able to use the birth control patch or vaginal ring instead. Like pills, these contain hormones and protect against pregnancy but need to be remembered less often. The patch is changed once a week, while the vaginal ring is changed once a month.
WARNING! If a woman taking the pill gets any of these signs, she should get medical advice right away:
- chest pain and shortness of breath
- strong headaches
- numbness in arms or legs
- strong pain in one leg
See more information about specific birth control pills.
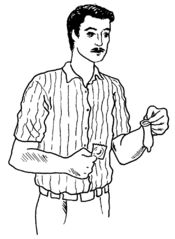
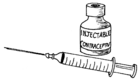
Injectable contraceptives
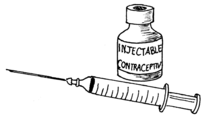
With this method, a woman gets a hormone injection to keep her from getting pregnant. Depending on the type of injection, protection lasts for 1 to 3 months
Injections are very effective. Very few women who use this method become pregnant. Another advantage to this method is that a woman does not have to do anything before having sex. And no one except her health worker needs to know she is using a family planning method.
The disadvantages are similar to those for birth control pills. In addition, many women who get injections have no monthly bleeding at all. These effects are not dangerous, but they may be uncomfortable. Another disadvantage is the woman must go to a health worker once every 1 to 3 months to get the injection. And like other hormonal methods, injections do not protect against HIV or other STIs.
Depo Provera and Noristerat injections contain only progestin, are given every 2 or 3 months, and are safe for women who should not use estrogen. If a woman is sure she is not pregnant, these injections can be started at any time and give protection in 7 days. They can be started the same day or any time within 7 days after birth, an abortion, or miscarriage and protect immediately.
Other injections (Cyclofem and Mesigyna) contain estrogen and progestin, and are given every month. If a woman is sure she is not pregnant, these injections can be started at any time and give protection in 7 days. They can be started the same day or within 7 days after abortion or miscarriage and protect immediately. Methods that contain estrogen increase the risk of blood clots and may limit how much breastmilk a woman makes. So women who are not breastfeeding should wait at least 3 weeks after giving birth before starting these injections. Women who are breastfeeding should wait 6 weeks (if partially breastfeeding) to 6 months (if exclusively breastfeeding) after giving birth.
When a woman stops getting injections, it may take longer than usual (as much as 3 to 9 months) for her to get pregnant. Women should always be told this before getting injectable contraceptives. For this reason, injections are best for women who are sure they do not want to get pregnant in the next year or more.
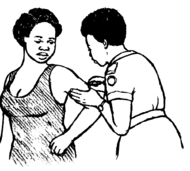
Implants
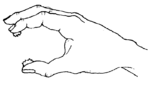
With this method, a trained health worker puts small, soft tubes under the skin of a woman’s arm. The implant then releases progestin and prevents pregnancy for 3 to 5 years, depending on the type of implant. Implants must be replaced after those 3 to 5 years are over. If a woman wants to get pregnant before that time, the implant must be removed by a health worker.
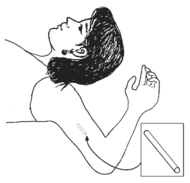 |
| Implants are put under the skin, and can be removed by a trained health worker. |
A woman with implants does not have to do anything before sex to prevent pregnancy. Implants only contain progestin — so they are safe for women who should not take estrogen. And they can be used safely while breastfeeding.
Implants have the same risks and side effects as other hormonal methods. Most women who use implants have very irregular monthly bleeding, with spotting and light bleeding between monthly bleeding. This usually gets better after a year of using this method. And like any hormonal method, implants do not protect against HIV or other STIs.
Implants can be started at any time and give protection in 7 days. They can be started the same day or within 7 days after birth, an abortion or miscarriage and protect immediately. A woman cannot remove implants herself. They can only be removed by a trained health worker. And it may be difficult to find a health worker who knows how to remove them. Women should understand this before the implants are put in.
WARNING! Watch women with implants for these signs of dangerous health problems. Get medical help if you find any of these signs:
- arm pain near the implant
- pus, redness, or bleeding around the implant
- the implant comes out
- monthly bleeding stops after being regular for several months
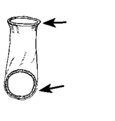
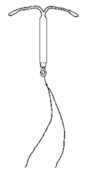
Intrauterine devices (IUDs)
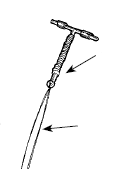
put inside
the womb
out of the
cervix into
the vagina
An IUD is a small device made of plastic that is put inside the womb to prevent pregnancy. The copper IUD prevents pregnancy for up to 12 years. Hormonal IUDs (Mirena and others) prevent pregnancy for 3 to 7 years, depending on the amount of hormone they contain. Once an IUD is put in, it stays inside the womb until it is taken out by a trained person. Chapter 21 explains more about IUDs and how to insert and remove them.
IUDs can be started at any time. The copper IUD gives protection immediately and hormonal IUDs give protection in 7 days. IUDs can be started the same day as or within 7 days after birth, abortion, or miscarriage. They protect immediately.
Usually, neither partner feels the IUD while having sex. A woman who uses an IUD does not have to do anything before having sex. And no one needs to know that the woman has an IUD inside.
Both types of IUDs can cause changes in monthly bleeding. The copper IUD can cause heavier monthly bleeding with more painful cramping for a few months. Rarely, this extra loss of blood can cause anemia. Hormonal IUDs can cause monthly bleeding to become very light or stop altogether, but they can also cause irregular bleeding and spotting.
These are some of the disadvantages and risks of IUDs:
- IUDs do not protect against HIV or other STIs.
- If a woman has chlamydia or gonorrhea when an IUD is inserted, the infection can spread to her womb. Womb infection can lead to infertility or other serious health problems. Make sure these infections are treated before having an IUD inserted.
- The woman cannot put in or take out an IUD herself. A health worker must do it.
WARNING! A woman with an IUD should get medical help if any of these danger signs appear:
- late or missed monthly bleeding
- pain in the belly that does not go away
- pain or bleeding during sex
- unexplained fever or chills
- unusually heavy bleeding from the vagina (soaking one or more pads or cloths in an hour)
A woman with an IUD must check every month to be sure it is still in place. The best time to check is after her monthly bleeding (or about every 4 weeks for someone using a hormonal IUD whose periods have stopped).
First, she should wash her hands. Then she should reach into the vagina with 2 fingers and feel for the strings of the IUD. They should be the same length each month.
If the strings seem shorter or longer or if she cannot feel them at all, the strings may have moved up into the womb or the IUD may have fallen out. In this case, the woman should use condoms or another barrier method until she can have the IUD checked by a health worker.
Abstinence and sex that does not cause pregnancy
There are many ways to have sex that do not cause pregnancy. Oral sex (mouth on genitals) and sexual touch (touching the genitals or other parts of the body) are both sexual activities that many people enjoy. They have very low risk of passing HIV and other STIs and they cannot cause pregnancy. Anal sex also cannot cause pregnancy, although it is much more likely than vaginal sex to pass HIV and other STIs.
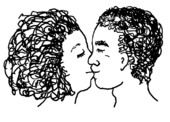
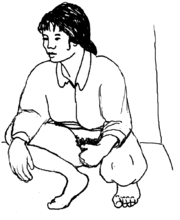
Abstinence means avoiding all sex that can cause pregnancy (sex with a penis inside a vagina). Abstinence is the surest way to prevent pregnancy, and can be a good way to reduce the risk of HIV and other STIs. However, in practice it can be difficult to maintain.
Breastfeeding to prevent pregnancy (Lactational Amenorrhea Method, LAM)
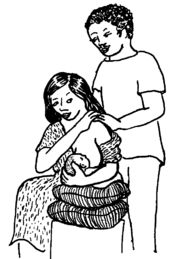
In the first 6 months after birth, most women who breastfeed do not release eggs from their ovaries, which means they cannot get pregnant when they have sex.
This method is most reliable if the baby is breastfeeding as often as he wants, including at night, and:
- the baby is less than 6 months old, and
- the woman has not had any monthly bleeding since giving birth, and
- the woman is giving the baby only breast milk.
The woman can easily get pregnant if she is giving the baby formula, water, or other drinks. She may get pregnant if the baby goes longer than 6 hours between breastfeeding times.
The breastfeeding method does not protect against HIV or other STIs. Also, getting infected with HIV while breastfeeding creates a danger of passing HIV to the baby. If there is any chance that the mother’s partner has HIV, they should use condoms each time they have sex, and get advice from an HIV prevention program.
Fertility awareness (natural family planning)
A woman can only get pregnant during her fertile time when an egg comes from her ovary into her tubes and womb — about once a month. To use fertility awareness, a woman must watch her body’s signs to understand when she is fertile. During the fertile time she and her partner must not have sex that can cause pregnancy (penis-in-vagina sex). At these times, they can try other types of sex like oral sex or sexual touching. Or they can prevent pregnancy by using condoms or a diaphragm during the fertile time.
Natural family planning costs nothing and has no side effects. But it can be difficult to use. Women do not always know when they are fertile, and if they have one irregular cycle, they can easily get pregnant. This method usually works best when couples receive training before using it. Natural family planning does not protect against HIV or other STIs.
Natural family planning does not work well for women who do not have control over when they have sex. During a woman’s fertile times, her partner must be willing to use condoms or a diaphragm — or not have sex that can cause pregnancy.
Women whose cycles are very different lengths each month should not use this method either. Women who recently gave birth or had an abortion should not use this method until their cycles are regular for several months.
There are many ways to use fertility awareness. In this book we talk about the mucus method and the counting days method. These methods work best when they are both used together. But one method alone is better than nothing.
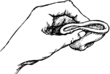
The mucus method
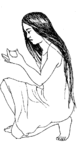
With the mucus method, a woman checks the mucus from her vagina every day to see if she is fertile. On her fertile days, the mucus is stretchy and slimy, like raw egg.
To check the mucus, a woman should wipe the vagina with a clean finger, paper, or cloth. Then she should look for mucus.
| Clear, wet, slippery mucus comes during the fertile time. Do not have sex that can cause pregnancy. |
 |
 |
White, dry, sticky mucus (or no mucus) comes during other times of the month. It is probably OK to have sex that can cause pregnancy 2 days after the first dry day. |
| After 2 or 3 months of practice, a woman can easily recognize these changes in her mucus. | |||
How to Use the Mucus Method
- Check the mucus at the same time every day. Check before having sex.
- Do not have sex that can cause pregnancy on any day you feel slippery mucus. Or use a condom or diaphragm on those days.
- Do not have sex that can cause pregnancy until 2 days after the last day that you have clear, slippery mucus.
- Do not douche or wash out the vagina at any time. This will wash the mucus away.
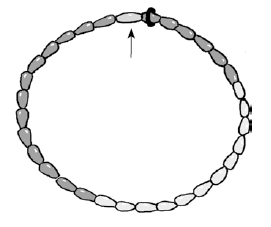
The counting days method (standard days method)
With the counting days method, a woman does not have sex that can cause pregnancy during any time that she might be fertile. This method can only be used by women with regular cycles that last between 26 and 32 days. This means that the time from the first day of one monthly bleeding to the first day of her next monthly bleeding must be at least 26 days, and no more than 32 days.
This method will usually work for a woman who has nearly the same number of days from one monthly bleeding to the next (regular cycles). But if a woman has one cycle of a different length, she can easily get pregnant. It is common for a woman to have a cycle of a different length when she is sick or feeling a lot of stress. When a woman is sick or feeling stress, it is best for her to use a different family planning method until she is well and her cycle is regular again.
How to use the counting days method
For this method to work, the woman cannot have sex that can cause pregnancy from the 8th day of her cycle through the 19th day of her cycle. If she does, she must use another method of family planning.
Sterilization
Sterilization is an operation that makes it almost impossible to have a baby. This method is permanent. It is only good for someone who never wants to have another baby.
These operations are done at medical centers. The surgery is fast and safe. Sterilization is almost always completely effective. A doctor can try to undo a sterilization, but that operation is expensive and often does not work.
Sterilization does not protect against HIV and other STIs.
Sterilization for men (vasectomy)
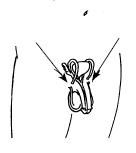
is made
here
here
A vasectomy is a simple operation. It takes only about 10 minutes. A health worker inserts a tool through the skin of the testicles to cut the tubes that carry sperm to the penis. The skin heals quickly and the testicles are not harmed.
The operation does not change a man’s ability to have sex or feel sexual pleasure. He still ejaculates (comes), but sperm cannot get from the testicles into the semen. For about 3 months, there are still sperm in the tubes, so the couple must use another method of family planning.
Sterilization for women (tubal ligation)
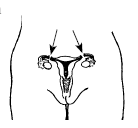
cut or tied
here.
Tubal ligation is a little more complicated than vasectomy, but it is still very safe. A health worker inserts a tool through the skin near the bellybutton to cut or tie the tubes that carry the woman’s eggs to her womb. The operation takes about 30 minutes. Tubal ligation does not change a woman’s monthly bleeding or her ability to have sex and sexual pleasure.
A method of sterilization called tubal occlusion (Essure, Adiana) places tiny metal and plastic coils in the Fallopian tubes to create scars that block the sperm from reaching an egg. It does not require surgery, but this method has generated many serious problems and is no longer available in some countries. No one should use it.
Emergency contraception: Pills
Emergency contraception is a way to avoid pregnancy after having unprotected penis-in-vagina sex. If a woman has sex without using a family planning method, and she does not wish to get pregnant, she can take a high dose of birth control pills as soon as possible — within 5 days of having sex. The sooner a woman takes the pills, the more likely they are to work.
This is not the best method to use every time a woman has sex. Emergency contraception contains more hormones than daily-use birth control pills, so it has more side effects. It is also more expensive than regular birth control pills, and less effective than other methods of preventing pregnancy.
| How to take pills for emergency contraception | ||
| Emergency pills containing 1.5 mg (1500 mcg) levonorgestrel (NorLevo 1.5, Plan B One-Step, Postinor-1) | Take one pill, one time only | |
| Emergency pills containing 30 mg ulipristal acetate (Ella, Ella-One) | Take one pill, one time only | |
| Emergency pills containing 0.75 mg (750 mcg) levonorgestrel (NorLevo 0.75, Optinor, Postinor-2, Plan B) | Take 2 pills, one time only | |
| Emergency pills containing 50 mcg ethinyl estradiol and 250 mcg levonorgestrel (Tetragynon) | Take 2 pills | Take 2 more pills 12 hours later |
| Combined pills containing 50 mcg ethinyl estradiol and 250 mcg levonorgestrel (Neogynon, Nordiol) or 500 mcg norgestrel (Ogestrel, Ovral) | Take 2 pills | Take 2 more pills 12 hours later |
| Combined pills containing 30 mcg ethinyl estradiol and 150 mcg levonorgestrel (Microgynon, Nordette) or 300 mcg norgestrel (Lo-Femenal, Lo/Ovral) | Take 4 pills | Take 4 more pills 12 hours later |
| Combined pills containing 20 mcg ethinyl estradiol and 100 mcg levonorgestrel (Alesse, Lutera) | Take 5 pills | Take 5 more pills 12 hours later |
| Progestin-only pills (minipills) containing 75 mcg norgestrel (Neogest, Ovrette) | Take 40 pills one time only | |
| Progestin-only pills (mini pills) containing 30 mcg levonorgestrel (Microlut, Microval, Norgeston) | Take 50 pills one time only | |
Emergency contraception: IUDs
Some IUDs can also be used as emergency contraception. A trained health worker must insert the IUD within 5 days of a woman having sex. All copper IUDs and a hormonal IUD that contains 52 mg of the hormone levonorgestrel will prevent a pregnancy. The IUD can then be left in to prevent future pregnancies. But this method should not be used by a woman who might have an STI.
Pulling out (withdrawal)
In this method, a man pulls his penis out of the woman’s vagina and away from her genitals before he ejaculates. This keeps most sperm from getting inside the vagina.
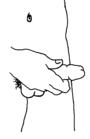
If a man is willing and able to pull out every time before he ejaculates, this method can work reasonably well. It costs nothing and is always available. But a man may not want to or be able to pull out before the sperm comes. This means the woman could get pregnant. Also, a woman may worry about whether the man will pull out in time, and feel less pleasure because of that worry. This method is more effective when combined with another method like spermicide or a diaphragm.
This method may give some protection against HIV and other STIs.
Contraceptive sponge
The contraceptive sponge is a round circle of foam that is soaked in spermicide. It should be wet with clean water before inserting it deep in the vagina with a finger. It should be left in place for at least 6 hours after sex but not longer than 24 hours. It can be removed by reaching in and pulling the attached loop. This method does not protect against STIs and should be used only by women who know their partner does not have HIV, as the spermicide in the sponge can irritate the skin of the vagina and allow the virus to enter the body more easily. Women may also get more yeast or bladder infections with this method.
New methods of family planning
New methods of family planning are being developed all the time, some for men too. These methods may only be available in some places and may be expensive. We include them here because the more people know about and ask for them, the more available and affordable they may become. Having more methods and methods that work differently allow people who want to prevent pregnancy to find a method that meets their needs.
Once-a-month birth control pills prevent pregnancy in the same way as minipills but they only have to be taken once each month. Some people are less likely to miss pills that need to be taken less often. This helps prevent unintended pregnancy.
A new kind of patch can be pressed on the skin right before sex and removed after only a few minutes. It uses a strong form of progestin. Unlike the combined hormonal patch currently available, this new patch is safe for people who cannot use methods with estrogen and it is more private because it is not worn all the time.
A non-hormonal gel inserted in the vagina just before sex makes the vagina acidic. This slows sperm movement and prevents sperm from reaching the egg.
A gel of progestin and testosterone prevents the testicles from producing sperm. It is rubbed onto a man's shoulders and arms once a day.
Vasalgel/RISUG is a gel that stops sperm from moving from the testicles to the penis. This prevents pregnancy in a similar way to a vasectomy, but is reversible. }}
Methods that do not prevent pregnancy
These common ways people try to prevent pregnancy do not work.
- Wearing charms will not prevent pregnancy. Neither will spells or prayers.
- Urinating after sex will not prevent pregnancy (though it may help prevent urinary tract infections).
- Washing out the vagina (douching) after sex does not prevent pregnancy. Some herbs or harsh chemicals used for douching can also injure the vagina.