Hesperian Health Guides
Learn how STIs spread to help prevent them
HealthWiki > Health Actions for Women > Chapter 5: Preventing Sexually Transmitted Infections (STIs) > Learn how STIs spread to help prevent them
Sexually transmitted infections are caused by different kinds of germs that live in a person’s blood, semen, or vaginal fluids. These germs are too small to see. STIs are passed from person to person only when an infected person’s blood, semen, or vaginal fluids get inside another person’s body through contact between the vagina, penis, or anus, or through cuts or sores in the skin. You cannot get any STI from touching a person in other ways, from sharing food or toilets, or from insect bites.
Unprotected sex. All STIs can pass from an infected person to another person if the couple has intercourse (man’s penis in a woman’s vagina) or anal sex (man’s penis in a woman’s or a man’s anus) without using a condom.
Oral sex. STIs can also pass from an infected person to another person if the couple has oral sex (putting the mouth on another person’s penis, vagina, or anus) without using a condom or a latex barrier between one person’s mouth and the other person’s genitals. HIV is rarely passed from person to person with oral sex, but other STIs such as gonorrhea, herpes, and HPV (human papilloma virus) can be passed easily this way.
All STIs can be passed during sex, but some can also be passed in other ways.
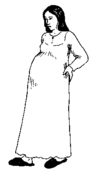
Mother-to-child. A woman can pass most STIs to a baby during pregnancy or childbirth. HIV is the only STI that can also be passed from a woman to a baby through breastfeeding.
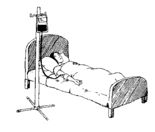
Blood transfusions. A person can become infected with HIV, syphilis, or hepatitis B or C through a transfusion of blood that has not been tested to prove it does not contain the germs that cause these infections.
Injections, skin piercings, or tattoos using unsterilized needles or sharp tools. A needle or sharp tool used to inject medicine or drugs, pierce the skin, shave, or tattoo a person with hepatitis B or HIV can pass those infections if it is used on another person. A new sterilized needle or tool should be used each time for injecting, piercing, shaving, or tatooing.
A person can have more than one STI at the same time. Having one STI often increases the risk of getting another one, because the infection weakens the body’s resistance to other STI germs. Discharge from the penis or vagina, or sores on the skin, make it easier for germs to get inside the body.
Contents
STIs pass more easily from a man to a woman
There are 3 main reasons why women’s bodies are more vulnerable to STIs than men’s bodies.
- The semen of a man with an STI contains more germs than the vaginal fluids of a woman with an STI, so a woman receives more germs when a man ejaculates or climaxes inside her than a man receives from putting his penis inside the woman’s vagina, anus, or mouth.
- When a man with an STI has unprotected sex with a woman and he climaxes inside her, his semen stays inside her body long afterward, so the STI germs have more time and favorable conditions for causing an infection in the woman. Rinsing the inside of the vagina after sex will not remove all of the semen.
- The skin of both the vagina and the anus is thin and easily cut or torn during sex, while the skin on the penis is thicker, so STI germs pass more easily through the skin inside a woman’s body than through the outside skin on the man’s penis.
Preventing STIs
Safer sex means ways of having sex that prevent or lessen the likelihood of STIs passing between partners. It means having as little contact as possible with the skin of your partner’s genitals and not letting fluids from your partner’s penis or vagina touch your genitals or mouth. Safer sex is more likely to happen when a woman is able to talk about sex with her partner and when communities promote conditions that empower girls and women, including through access to education and health services for the testing and treatment of STIs.
How sexual networks spread infections
Understanding how certain patterns of sexual relationships spread STIs can help people understand the importance of preventing STIs in every relationship. Many women want to believe that they can protect themselves by being faithful to their husband or partner. But this works only when both partners are faithful and do not have any infection when they first start to have sex together.
This activity can help people see how an infection can spread through a whole community, even if only some people have more than one sexual partner.
Activity
Handshake game
This activity uses HIV as an example, but all STIs can spread the same way.
To prepare, gather a small piece of paper for each person. Draw a circle on 3 papers. Draw an X on 1 paper. Leave the others blank. Fold the papers to hide the markings.
- Mix the papers up and give one to each person. Ask everyone to look at her own paper but not at anyone else’s.
 Hello. Let me shake your hand.I’d like to shake your hand, too!
Hello. Let me shake your hand.I’d like to shake your hand, too! - Ask the participants to walk around and shake hands with 3 people and then sit down.
- Ask the person with the X on her paper to stand up. Ask everyone who shook hands with that person to also stand up. Ask anyone seated who shook hands with anyone standing to stand up too. Repeat this until everyone is standing.
Explain that for this activity, the X represents HIV and shaking hands with the person holding the X meant having unprotected sex. This means that all the people standing might now have HIV.
- Ask those with a circle on their papers to raise their hands. Explain that the circle is a condom, so the people using condoms were protected from HIV and can sit down.
- Discuss the activity. You might ask questions like these:
- How did the person with the X feel to find out this meant having HIV?
- How did everyone feel when they had to stand? How is this like a person finding out he or she had sex with someone who has HIV?
- When you learned the circle represented a condom, did you feel relief? Did it make you glad you had used a condom?
- Collect all the papers and pass them out again. Do the activity again, but this time give some choices anyone can use for preventing the spread of the infection.
- No sex at all ― the person does not shake hands.
- Use a condom ― have some plastic bags or socks people can use to cover their hands.
- Have only one partner who has no infection and has sex only with you ― shake hands after looking at each other’s papers and stay together without shaking anyone else’s hand.
- Be sexual in ways that do not share body fluids, such as giving pleasure by using hands ― touch fingertips or elbows instead of shaking hands.
- After the activity, ask the person with the X to stand up again. Then ask people to stand up if they shook hands with that person without covering their hands.
- Ask anyone who did not stand to say what action they took to protect themselves.
- You might also ask whether it was difficult or uncomfortable for anyone to "use protection" while shaking hands. Why? Would it become more comfortable with time? Or if they had a single, faithful relationship, was that difficult? Why?
- Discuss what makes it easier or more difficult to talk about STIs with a partner.
- How would you feel if someone you had sex with told you that he or she had an STI? Is it better to know or not know? Why?
- If you think it is better to know, how can you make telling someone easier?
- What can you know for certain about a sexual partner? What can you not know for sure?
Facts about STIs
Discussing the health problems caused by STIs that go untreated can help everyone understand the importance of seeking treatment and of preventing the spread of STIs in the first place. Here is some general information about different STIs. You can find out more in Where Women Have No Doctor or by speaking with a health worker.
| Gonorrhea and chlamydia are easy to cure if treated early. If not, they can cause serious infection and infertility in both women and men, and serious problems for a baby during both pregnancy and childbirth. |
|
Signs in a woman: she may have no signs at all, or they may not appear for several weeks after sex with an infected person. There will be discharge from the vagina, lower belly or pelvic pain, fever, and pain when passing urine. Oral sex with a man who has gonorrhea can cause a sore throat with pus or swollen neck glands. Signs in a man: often no signs, or signs may appear 2 to 5 days after sex with an infected person. There will be discharge from the penis, pain when passing urine. These infections can also affect a pregnancy by causing early labor, low-weight babies, baby dying in the womb (stillbirth), or early infant death. In a newborn baby they can also cause pneumonia and eye infections leading to blindness. A woman can also get a womb infection (pelvic inflammatory disease), or a baby can grow outside the womb (ectopic pregnancy), which can lead to infertility and even death. |
| Syphilis is an STI that has effects throughout the body and can last for many years. It can be cured with medicine if treated early, but will lead to serious illness and death if not treated. |
| Signs in a woman and man: a soft painless sore (chancre) on the genitals that may look like a blister or an open sore. Syphilis does not affect fertility, but it can cause early labor, low-weight babies, baby dying in the womb (stillbirth), or early infant death. Also, the baby may be born with syphilis, leading to severe illness and death. |
| Trichomoniasis (trich) is a very uncomfortable and itchy STI that can be cured if treated. Women and men often do not have any signs. |
| Signs in a woman: unusual bad-smelling discharge from the vagina, with red and itchy genitals, and pain or burning when passing urine. Fertility in both women and men can be affected, and a baby girl can be born with a vaginal infection. Rarely, a baby may develop problems when passing urine, and have trouble breathing. |
| Chancroid causes painful sores on the genitals or anus that bleed easily and swollen glands (buboes) in the groin. It is easily confused with syphilis. It can be cured with medicine. |
| Herpes (HSV, genital herpes) is caused by a virus. There is no cure for herpes but there is treatment to make a person feel better. |
| Signs in a woman or man: none, or during the first infection, may feel severe burning and itching in the genitals followed by small painful blisters like drops of water on the genitals that burst open and form painful open sores, along with feeling ill, like having the flu. After the first infection, a sore will appear in the same place over and over, but may be milder. If a woman is pregnant and it is a first infection, herpes may cause a baby to die in the womb (stillbirth), a severe infection in the baby, or problems in the development of the baby’s brain and nervous system. |
| Hepatitis B (hep B) cannot be easily cured because the medicine is expensive and often not available, but it can be prevented with a vaccine. |
| Signs in a woman or man: none, or fever, fatigue, yellow eye or skin (jaundice), dark urine, and whitish stools. Hep B can affect fertility and pregnancy if there is serious damage to the liver, and can cause liver disease and cancer. A baby born to a woman with hep B may also get the disease. |
| Human Papilloma Virus (HPV, warts) are small, painless bumps that have a rough surface and can be removed, but not cured. |
|
Signs in a woman: the bumps appear on the outside (vulva) and inside of the vagina, and around the anus. Warts may grow larger and bleed during childbirth, and a c-section may be required. Rarely, warts can pass to a baby during childbirth. Signs in a man: the bumps appear on or inside the penis and around the anus. Some types of HPV that can cause cancer of the cervix or penis can be prevented with a vaccine. Regular cervical cancer tests for women can help find early signs. |
| Human Immunodeficiency Virus (HIV) has no cure, but treatment can help people with HIV live longer and in better health. |
|
Signs in a woman or man: none, or 2 to 4 weeks after contact a person may feel ill, like having bad flu, diarrhea, fever, swollen lymph nodes, and weight loss. HIV does not affect fertility, but it may cause early labor and can be passed to a baby during pregnancy, birth, or breastfeeding, so testing is important. |
Testing and treatment are essential
Most STIs can be in a person’s body without showing any signs. This means that a person can have an STI and pass the infection to others without knowing it. It also means that many women have serious womb infections, ectopic pregnancies, miscarriages, and other health problems caused by STIs that went untreated, because the women didn’t know they had an infection.
One way to stop STIs from spreading is for women and men to get treated as soon as they have any signs and make sure their partners get treated at the same time. STIs can be treated with medicines, but a person can get infected again after treatment if she has unprotected sex with a partner who has an STI.
Women and men should also get tested every 6 to 12 months if they have unprotected sex with more than one partner, if they think their partner may have sex with other people, or if they or their partner injects drugs such as heroin. Some tests use a blood sample; others use a sample of fluid from a woman’s vagina or a man’s penis, or a sample from a person’s mouth.
Routine testing helps lessen the stigma of STIs
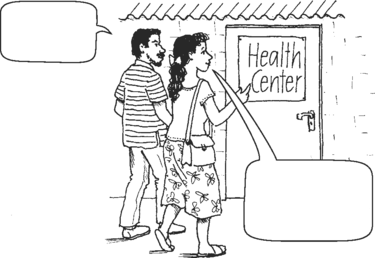
Health centers can help lessen the stigma of having an STI by providing testing and treatment as a routine part of health care for both women and men. For people to be comfortable getting tested for an STI, they need to trust that they will be treated with respect and privacy.
Some health centers do provide STI testing and treatment as part of family planning services and regular pregnancy check-ups. When men accompany women on these visits, health workers can encourage them to get checked and treated for STIs. This means the woman does not have the extra burden of telling her partner and making sure he gets treated.
"Wellness check-ups" take the stigma out of STI testing and treatment
Most people in Papua New Guinea live in rural areas far from health centers. STIs are very common in these communities, because many people do not know about prevention and cannot easily get tested and treated for infections. Many women suffer from pelvic inflammatory disease (PID), a serious infection of the womb that is often caused by untreated STIs. PID often causes infertility, so a woman who has had it may never be able to get pregnant and have children. Infertility can be very sad for any woman, but infertile women in Papua New Guinea may be isolated from the community and beaten by their partners.
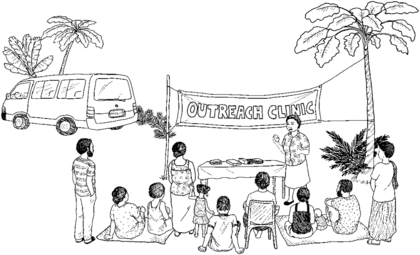
Marie Stopes International provides STI counseling, diagnosis, and treatment to rural communities through mobile outreach teams. These teams of 2 or 3 heath workers travel to remote parts of the country carrying the equipment they need in small vans. By helping people understand how infertility can be caused by STIs, these teams help motivate people to practice safer sex and get tested for STIs.
This program is successful in part because it brings information and services directly to people in their communities. But it is especially successful because STI services are included in "Wellness check-ups" for men, women, and youth. This makes it easier for young people and unmarried women to have access to family planning and STI services as part of general health check-ups.
The outreach teams are also well received, because they provide services without judging people’s customs or relationships. In the highland region, where polygamy is common, clients are provided with treatment for all sexual partners in the marriage, if they choose.


