Hesperian Health Guides
Chapter 19: Bone Infections: Osteomyelitis
Chronic (long-lasting) bone infections are fairly common in villages where persons go barefoot and where injuries and illnesses that can lead to bone infections are frequent. They can be caused by fungus, or by many different kinds of bacteria (including typhoid, tuberculosis, and staphylococcus). Often these infections last for years, causing bone destruction and severe disability.
Bone infections are a very common complication of injuries, burns, and pressure sores in persons who have no feeling in their hands and feet. This includes persons with spina bifida, spinal cord injury, and leprosy. Because the person does not feel pain, often she does not rest, clean, or protect the injured area. As a result, it becomes infected. Gradually the infection gets deeper until it reaches the bone.
Through proper early care of sores and injuries, bone infections can usually be prevented.
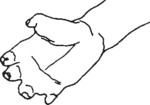
The loss of parts of the body sometimes seen in a person who has leprosy (Hansen’s disease) is not caused by the leprosy germs. It is caused by other germs, which infect the bone because of injuries the person gets that are not cared for because they do not hurt.
Signs of chronic bone infection
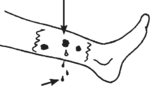
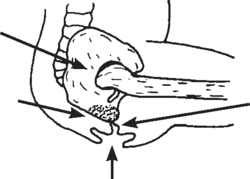
- The skin near a bone has small, deep sores that heal and then open again to drain pus. Gradually the affected area gets bigger and new holes open.
- There may or may not be pain.
- The pus may or may not smell bad.
- Usually there is no fever—except sometimes at first or at times when the infection gets into the blood.
- Often the infection will get better with antibiotics, but keeps coming back.
- The affected bone may gradually become thicker as it is destroyed inside and forms a new bony covering.
Treatment
- Get experienced medical help. Bone infection requires treatment with multiple antibiotics in a vein for several weeks. If possible, a sample of the pus should be studied (cultured) by a medical laboratory to find out what kind of infection it is and what medicine is likely to work best.
- Surgery may be needed to remove the dead, infected bone. Doing this in a timely manner may prevent the need for amputation.
- Sometimes amputation is necessary.
- Even with treatment, after months or years without symptoms, new sores may open and again begin to drain from the infected bone.
Rehabilitation and aids
 |
| Large hole down to the bone in the foot of a woman with a bone infection (osteomyelitis). She has had this problem since childhood 30 years before. |
What kind of rehabilitation or orthopedic aids may be needed will depend on the amount of destruction that has occurred. Sometimes surgery cannot be obtained or the person may prefer to live with the injuryrather than with an amputated limb.
For prevention, rehabilitation, and aids, see chapters 24, 26, and 58 on pressure sores, leprosy, and braces.
When there has been a lot of bone destruction, sometimes a brace can help make walking easier.